The final nail in the coffin of manual thrombo-suction (MT) during treatment of acute STEMI has been delivered in this week’s ‘TOTAL” trial published in the NEJM. The TAPAS study had in randomized manner shown reduced mortality with MT some years ago in a cohort of more than 1000 patients of STEMI followed for a year. Manual thrombo-suction was considered effective and safe and therefore widely practiced during primary PCI. The procedure was simple, inexpensive and intuitively appeared to produce excellent results. TAPAS (a single center study) was however underpowered for hard clinical endpoints and their results were reckoned hypothesis generating.
The randomized Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia (TASTE) trial however cast many doubts over the TAPAS study. TASTE did not record any significant improvement in all-cause mortality, hospitalization for MI, or the risk of stent thrombosis at the close of one year with catheter based thrombus aspiration with PCI in STEMI. The patients came largely from Sweden but also from Denmark and Iceland. The Scandinavian trial with MT came on the heels of the TAPAS trial that had compared primary PCI with and without MT in patients of STEMI and reported significant improvement in myocardial perfusion and survival after a year of follow-up. The results of TAPAS were not replicated by TASTE that randomized 3621 patients to MT with primary PCI and 3623 patients to primary PCI alone. The investigators of TASTE concluded that routine aspiration before PCI in patients with STEMI did not reduce rate of death or the composite of death from any cause, MI or stent thrombosis at 1 year (hazard ratio, 0.94: 95% CI, 0.80 to 1.11; P=0.48). Their paper was published in September 2014 by the NEJM.
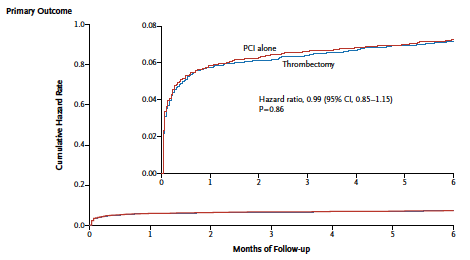
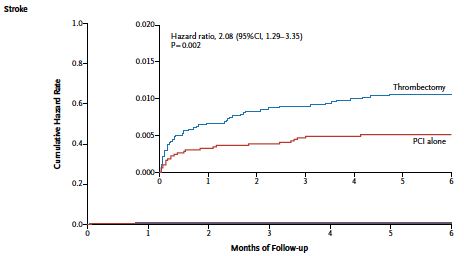
Now yet another large randomized trial has reported that routine MT as compared to PCI alone does not reduce cardiovascular death, recurrent myocardial infarction, cardiogenic shock, or NYHA class IV heart failure within 180 days, but was somehow associated with increased stroke at 30 days. The TOTAL trial randomly assigned 10,732 patients with ST-segment elevation myocardial infarction undergoing primary PCI to a strategy of routine upfront MT versus PCI alone. Manual thombo-suction before deployment of a stent during primary PCI in a STEMI patient appears logical because removal of the thrombus manually by a catheter has the potential of mitigating distal embolization and improvement in micro-vascular perfusion. TOTAL did record improved ST-segment resolution and distal embolization with MT but this was not translated to clinical benefits.
The increased rates of stroke in TOTAL are not easily explained (1% in the thrombectomy versus 0.5% in the PCI alone cohort,; there were however no increased stroke rates in the TASTE study with manual thrombo-suction in patients with STEMI. The thrombectomy procedure followed in TOTAL consisted of crossing the lesion with a wire, the thrombectomy catheter was advanced over the wire and suction begun before the device crossed the lesion, if the operator was unable to cross the lesion with the thrombectomy catheter pre-dilatation with a small balloon was permitted, the guiding catheter was to be fully engaged with the ostium of the culprit vessel during MT to prevent systemic embolization, and after thrombectomy the guide catheter was to be aspirated to ensure removal of air or thrombus.
Initial thrombus size was graded as 0= no thrombus present; 1- possible thrombus present; 2= definite thrombus present (0.5 X vessel diameter); 3=definite thrombus (0.5-2 X vessel diameter); 4= definite thrombus present (>2 X vessel diameter); 5= total occlusion. Clinical primary composite outcome was 7.3% in MT group versus 7.5% in PCI alone group when thrombus size was >4. Primary outcome was 5.3% in the MT group versus 4.8% in the PCI alone group when thrombus size was <4 (p value was insignificant for interaction). Similarly there was no significant difference of results in other subtypes as age more or less than 65 years, anterior or inferior STEMI, the initial TIMI flow in infarct related artery, and symptoms of less than 6 hours or 6 to 12 hours.
The take home for now is that a strategy of PCI alone with only bailout thrombectomy should be the procedure of choice in patients with STEMI regardless of the intuitive appeal of the interventional cardiologist.