An interesting article recently published dilates on the fact that a drug backed by solid evidence in the past may be found ineffective some years later. Beta blockers considered indispensable subsequent to an acute myocardial infarction are now not recommended in post MI patients with normal left ventricle function. A beta blocker does not improve clinical outcomes in a post MI patient who does not have an impaired left ventricle. Another drug seems to be fizzling out as a prophylaxis against cardiovascular events. Three randomised trials have shown little or no benefit in clinical outcomes with prophylactic aspirin. In fact prophylactic aspirin is almost always associated with increased bleeds, which can be a serious advert effect. Some years ago however aspirin had consistently demonstrated good efficacy as a prophylactic in middle aged people. Prophylactic aspirin was backed by reasonably good evidence of better clinical outcomes. Why does the same medicine at the same dosage not work any longer? The explanation is simple; over the years population has altered, people are more health conscious now with much better lifestyle application. Also there is much greater emphasis on control of high blood pressure and management of lipids with statins. The net result is that the marginal albeit clinically significant prophylactic advantage has evaporated. Evidence based medicine is not forever, there can be an expiry date.
More commonly we are confronted with lack of data buttressing a drug or a device. The classic example is the intra-aortic balloon pump (IABP), which has been around for almost 40 years or more. The first time I used one was 37 years ago for a patient in cariogenic shock, we still lost the patient. Randomised data on IABP is restricted to cariogenic shock accompanying acute myocardial infarction. The SHOCK trials failed to show improved survival with the IABP; mortality persisted at 40% by 30 days. The employment of an IABP in patients with heart failure and low blood pressure was never tested in a randomised manner till the ‘ Primary intra aortic balloon support versus inotropes for decompensated heart failure’ randomised trial published last month (Eurointervention 2019;15: May). This Dutch trial although randomised trial is too small in size to be considered anything more than a pilot study. Only 32 patients were enrolled. Also this is a single centre trial. Simply put an IABP inserted right away performed better than an inotrope (INO) in patients with decompensated heat failure and low output (DHF-LO). All 32 patients were in their 50’s, had a mean blood pressure around 70 mm Hg, two thirds were male, two thirds had non ischemic heart failure, with an average respiratory rate of 23/m and mean mixed venous oxygen saturation ranging from 40 to 46%. No patient was suffering from acute coronary syndrome.
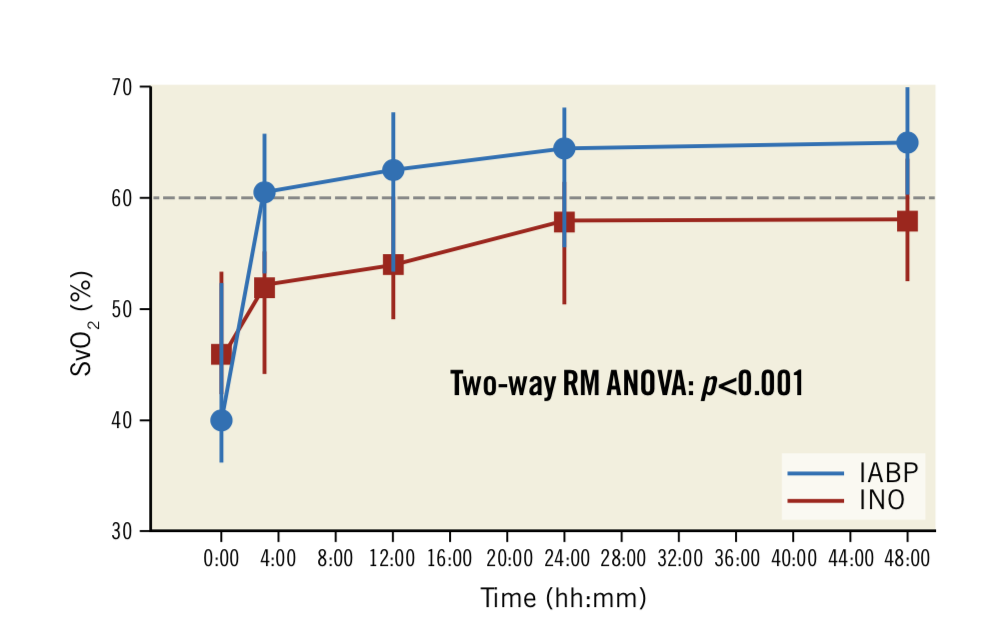
The trial compared IAB P use and inotropes as first line treatment for non ischemic DHF-LO. Remarkably the IABP patients immediately achieved a venous oxygen saturation greater than 60% as compared to p[atiemts provided inotropes ( dobutamine or enoximone). This benefit was sustained for more than 3 hours, also IABP patients were more responsive to diuretic treatment. Fall in NT pro BNP was significantly more, dyspnoea score better, and fluid retention lesser with IABP.
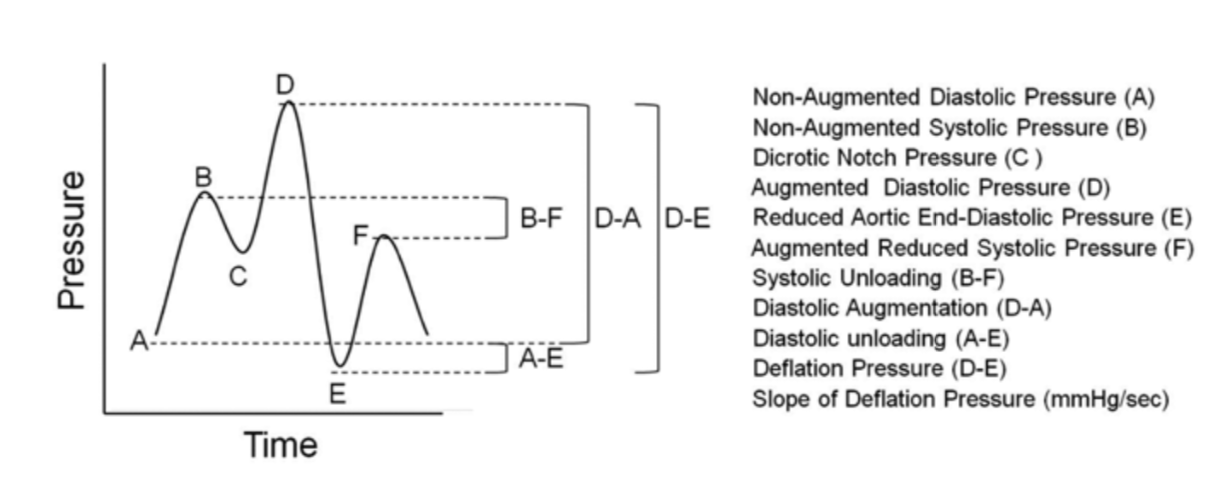
The researchers used 50 cc balloons instead of the 30cc or 40cc balloons as its has been shown that the 50cc balloon provides better haemodynamic support. By inflating only in diastole the IABP balloon reduces after-load, reduces oxygen consumption by the left ventricle, increases coronary artery blood flow and also increases cardiac output albeit by just a litre. The researchers emphasise that the IABP did not result in any serious adverse effect. The 30 day mortality was 23% in the IABP group versus the 44% in the inotrope group. The conclusion was that primary circulatory support buy IABP shoed significant increase in improved organ perfusion assessed by mixed venous oxygen saturation.
Advanced mechanical support that can augment cardiac output apart from IABP com in the form of Impella or as extracorporeal membrane oxygenation (ECM). However these systems are far more invasive, complicated too employ and without data clearly showing superiority to IABP. To repeat early implantation of an IABP in patents with decompensated heart failure and low output provided more effective treatment than inotropic agents. ECMO is still used in less than 3% of patents in the USA, largely because it is both incredibly expensive and invasive. Impella too is far more expensive than an IABP and leaves behind a much bigger hole in the femoral artery. Moreover all randomised trials comparing Impella with an IABP have failed to demonstrate a difference in clinical outcomes.
This small study needs to be confirmed by a larger randomised trial at the earliest. An IABP can be inserted in less than 5 minutes by an experienced operator plus it is far less expensive than the Impella or ECMO. Till then it may be worthwhile to use IABP in patients with decompensated heart failure patients not suffering from acute ischemia. Inotropes on the contrary increase contractility of the left ventricle but also increase heart rate and oxygen consumption; increasing risk of arrhythmia and worse mortality.The benefit of intra-aortic balloon counterpulsation treatment in severe heart failure and low cardiac output remains largely unexplored.