One of the most dramatic and important achievements of the last century was the discovery of insulin in 1921-1922 in the University of Toronto. The patent remarkably got to be sold for a mere one dollar. Today a single vial of long acting insulin analogue costs almost $ 200 in the USA. North America has 7% of the world’s diabetic population but accounts for more than 50% of insulin sale, whereas China accounts for 25% of the world diabetic population but accounts for only 4% of insulin sales. Insulin sales could have been worth more than 20 billion dollars worldwide last year.
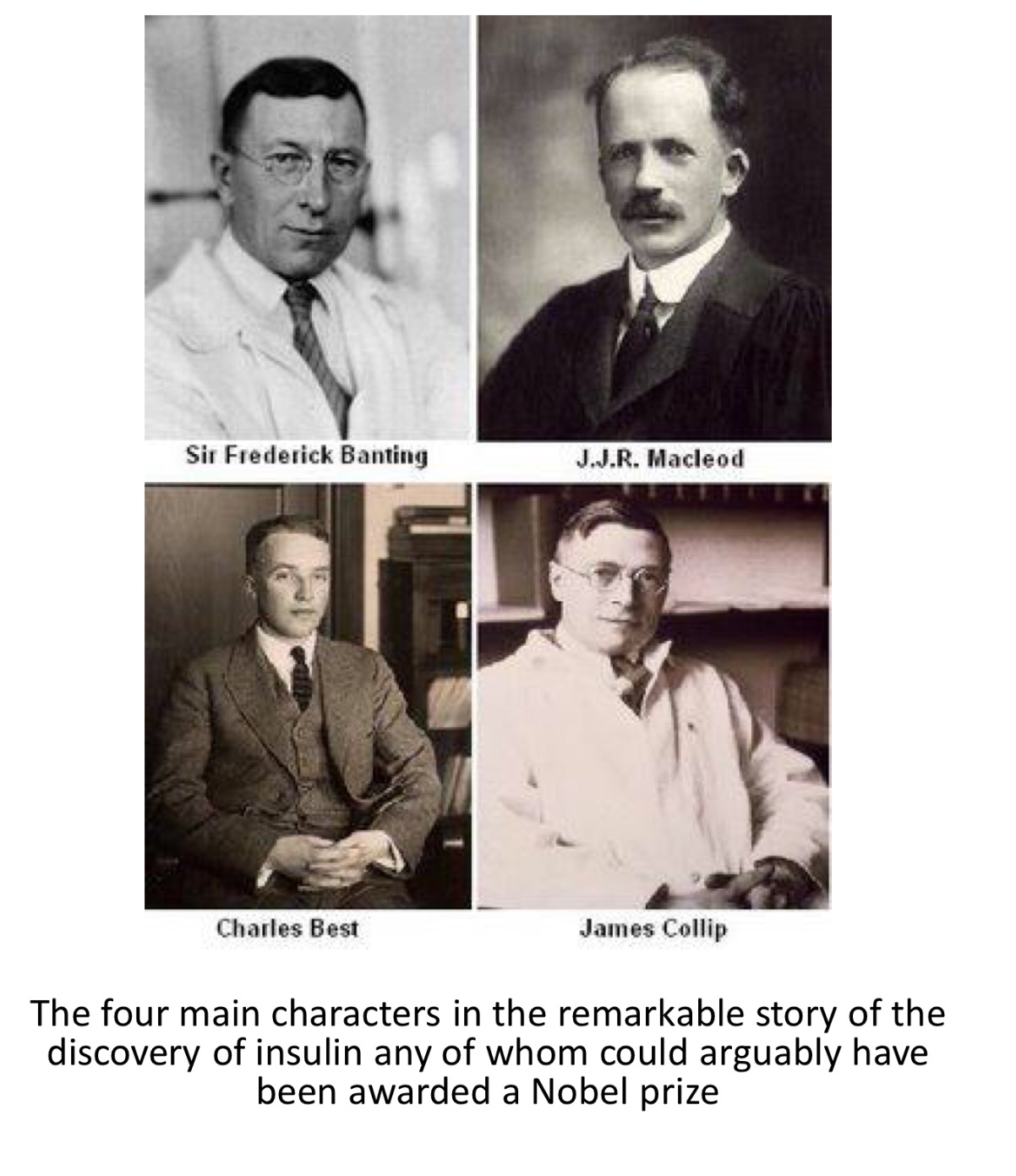
The story of the discovery has garnered a mythical hue. A 29-year-old surgeon Frederick Banting was assisted by undergraduate student named Charles Best in experiments with dogs that resulted in a crude insulin extract. The laboratory facilities were provided by the respected physiologist J.J.R. Macloed.The crude extract was refined by J B Collip, a biochemist. The crude insulin extract was injected in the first patient of diabetes in January 1922. This resulted in mild lowering of blood sugar, but the result was exciting enough for Eli Lilly in the US and Connaught Labs in Canada to begin industrial production of the wonder drug that would prove a life saver for patients of type 1 diabetes.
In 1923 the Nobel Prize in Physiology or Medicine was awarded to Banting and Macloed (but not to Best nor Collip). The 2 award winners went on to publicly share the prize money with Best and Collip. Michael Bliss wrote a remarkable and probably the best book on the discovery of insulin called “The Discovery of Insulin”. This is a book that should be read by any physician interested in the treatment of patients of diabetes, because having diabetes was a horror story before the discovery of insulin. It is difficult to comprehend life before the discovery of insulin.
Human insulin was introduced in 1982 (cost $14) and then insulin analogues in 1996 at $24 per vial. But today a vial of insulin analogue is out of the reach of a lot of American patients. The costs are mercifully less in India, which has the second largest population of diabetes in the world after China. Insulin glargine costs almost Rupees 600 while the ultra-longacting Degludec costs a little more than Rupees one thousand eight hundred. On the other hand synthetic human insulin, substantially cheaper, have almost been discarded in the USA. More over drug companies manufacturing insulin analogues are aggressively marketing the more expensive analogues in conventions and also getting studies published in premier medical journals.
A vial of neutral protamine Hagedorn (NPH), human regular (R) insulin, premixed 70/30 NPH sells for less than $25 in the US and even less in India. Combative marketing by drug companies is capable of driving physicians away from the proven efficacy of human insulin, at least in type 2 diabetes. Insulin analogues do not improve glycemic control nor reduce the risk of hypoglycemia as compared with human insulin. Human insulin can be as effective as the analogues if used skillfully and judiciously.
There are some differences of course between human insulin and the insulin analogues. The long acting insulin analogues have constant plasma levels for more than 24 hours, while human N insulin does not cover more than 18 hours. Nocturnal hypoglycemia is modestly less than human insulin in patients with type 2 diabetes. The challenge for the physician is to never be too aggressive in lowering the glycated hemoglobin levels (HbA1C). All insulin analogues are available in the pre filled pen forms while most human insulin are not. It matters little where a rapid onset insulin analogue is injected in the human body. In the case of rapid R human insulin the quickest onset of action is obtained with an injection in the abdomen.
The starting dose of bedtime human N insulin is usually 10 units (0.2 U/Kg of body weight) while premixed 70/30 human insulin should be started at 0.3 U/Kg. The premised version can be used twice a day keeping in mind that the chances of hypoglycemia are highest at mid day or mid night. The dose of an insulin analogue should be reduced by 20% if a switch is to made to human insulin. It is the considered opinion of quite a few dialectologists that many patients with type 2 diabetes can be safely treated with human insulin instead of the far more costly insulin analogue without compromising significantly on efficacy and safety. But as mentioned earlier the drug companies persist with their publications.
The latest study to be published is the DEVOTE research comparing safety and efficacy of insulin degludac insulin (ultra long acting ) versus insulin glargine (NEJM 12 June 2017). The researchers randomized 7637 patients of type 2 diabetes to receive either insulin degludac or insulin glargine at night. The primary composite clinical outcome of death from cardiovascular causes, non-fatal myocardial infarction, non fatal stroke, did not differ in the 2 groups at 24 months (8.5% in degludac versus 9.3% in the glargine group). More than 85% of these patients had established cardiovascular disease, chronic kidney disease or both. The mean duration of diabetes was 16 years and mean age of patients was 65 years. The authors concluded that in type 2 diabetic patients with high cardiovascular risk, degludac was non inferior to glargine where cardiovascular outcomes were concerned but had slightly less hypoglycemia by 1.7 absolute percent.
It would do well to remember the study by the ORIGIN trial investigators published in 2012 which randomized 12,537 people (mean age 63 years) with cardiovascular risk factors plus impaired fasting glucose, impaired glucose tolerance, or type 2 diabetes to receive insulin glargine or standard care. The rates of cardiovascular outcomes were similar in both groups after a follow up of 6 years. Insulin glargine however increased hypoglycemia and modestly increased weight. So we now know that cardiovascular outcomes may be similar in patients with type 2 diabetes accompanied by cardiovascular disease regardless of whether they are provided standard care or insulin glargine. We also know by the latest degludac trial that degludac is not superior to glargine.
So after 20,000 patients with type 2 diabetes having been randomized to standard care and the newer insulin analogues we can draw a plausible conclusion that most type 2 diabetes patients can me effectively managed with the older human insulin that are as affective and safe as the analogues apart from being significantly cheaper. The diabetic patient of the type 2 variety should however never be hesitant in beginning insulin therapy if needed , but must especially if a new patient of diabetes focus on exercise and a low calorie diet. Type 2 diabetes is a progressive disease and most if not all patients require a cocktail of exercise, diet, oral hypoglycaemic drugs and insulin. Almost 90% of patients of diabetes are type 2. Every patient with type 1 diabetes needs insulin for sheer survival. It is therefore imperative that insulin is made affordable to patients in need of it.