The Mayo Clinic has published a paper on the surgical approach in patients hypertrophic obstructive cardiomyopathy (HOCM) accompanied by mitral regurgitation (MR). The study has confirmed what is already well known that MR in HOCM is dependent upon systolic anterior motion (SAM) and in most patients this can be corrected by extended myectomy alone.
Hypertrophic cardiomyopathy (HCM) is characterized by asymmetrical myocardial hypertrophy plus fiber fibrosis and disarray. About one third of HCM patients have resting left ventricular outflow tract obstruction (LVOTO) with >30 mm gradient at rest. Another third have a resting gradient < 30 mm but obstruction can be triggered by exertion, increased myocardial contractility or afterload.
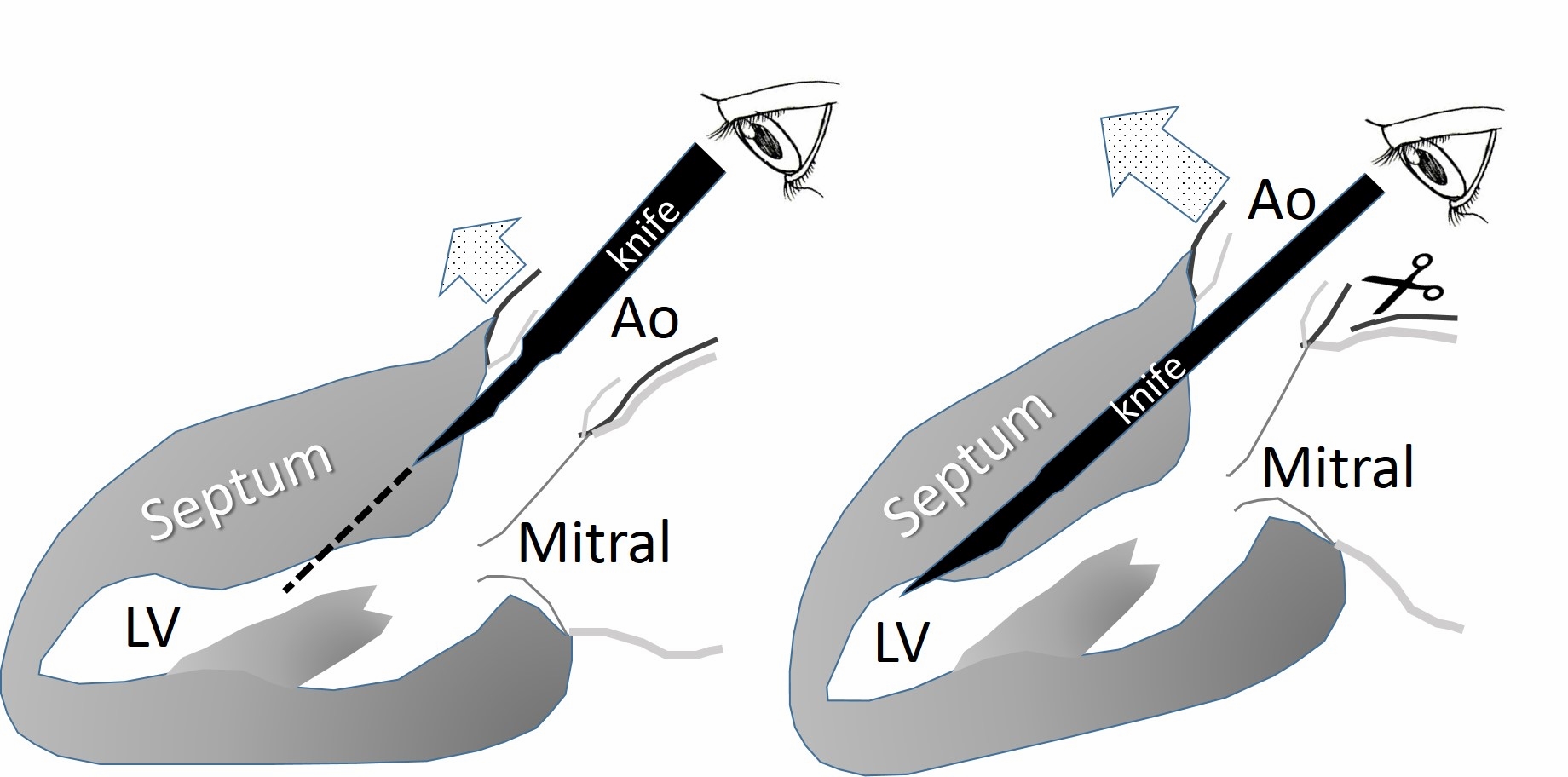
Dynamic LVOTO is caused by the combination of a hypertrophied septum and SAM of the mitral valve, which allows contact of mitral valve (MV) leaflets with the interventricular septum. Distortion of MV leaflets during SAM leads to mitral regurgitation (MR). The Morrow myectomy performed through an aortotomy involves resection of septal muscle about 1 cm beyond SAM contact, retaining 8-10 mm of residual septum. This is a blind procedure.
Primary structural abnormalities of the MV apparatus are common in HCM patients independent of obstruction; these include elongated MV leaflets, abnormal chordal attachments, and papillary muscle abnormalities. These abnormalities of the MV apparatus induce SAM aided by a venturi effect during systole. Adequate myectomy however is enough to treat MR in most HOCM patients. The Mayo Clinic Clinic data shows that in 2000 patients of HOCM, more than 90% underwent myectomy alone. Mitral regurgitation was corrected in 98% of these patients ( J Am Coll Cardiol 2016; 68:1497-504).
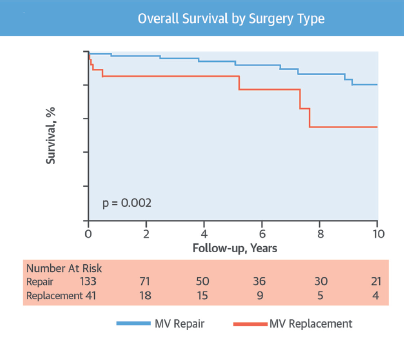
Concomitant MV intervention was required in about 9% of patients of whom 57% had a MV surgery prior to myectomy because of intrinsic abnormalities. The remaining patients had MV abnormalities discovered during myectomy and 87% % of these were treated by MV repair, while 13% underwent MV replacement. There were 75 patients with intrinsic MV abnormalities detected intraoperatively. Late survival was better with MV repair versus MV replacement.
Residual MR after myectomy was the result of incomplete extension of myectomy to the apex or due to iatrogenic damage (<1%).
Results of myectomy for HOCM depend upon the experience at the center performing the operation. The US records mortality as high as 5.9% nationwide while it is as low as 0.4% at HCM dedicated centers. The Mayo Clinic researchers have demonstrated that concomitant MV intervention should be done only in patients with intrinsic MV abnormalities or with iatrogenic damage to the valve. In the vast majority of HOCM patients extended myectomy is the only treatment required to relieve LVOTO and significant MR.
The paper concludes that in most HOCM patients, MR related to SAM is corrected by adequate myectomy alone. Concomitant MV surgery is rarely necessary unless intrinsic MV disease is present, and if needed repair because of improved term survival is preferred to MV replacement. Patients of HCM with obstructive element have reduced survival. In the absence of intrinsic MV disease, MR due to SAM regardless of severity decreases significantly with myectomy in the majority of patients.
Extended myectomy is performed first in patients without intrinsic MV disease and then MR is assessed by transesophageal echocardiography after discontinuation of cardiopulmonary bypass. The most common cause of residual MR or recurring LVOTO is because of inadequate myectomy.