The leading cause of kidney failure across the planet is type 2 diabetes. Patients with diabetes who develop reduction in estimated glomerular filtration rate (eGFR) to less than 60 mL/min per 1.73 m2 or albuminuria, or both over a period of 3 months, are considered to be suffering from chronic kidney disease (CKD). A ratio of urinary albumin (mcg/L to creatinine (mg/l) of less than 30 is normal, a ratio between 30-300 suggests microalbuminuria, and a value greater than 300 is macroalbuminuria. A patient with diabetes and also CKD has a much graver prognosis than a patient of diabetes without CKD. Herein lies the importance of regularly checking for eGFR and morning urinary albumin creatine ration (UACR) because the aim of treating diabetes kidney disease is to reduce albuminuria and progressive reduction in eGFR. Blocking the renin-angiotensin aldosterone system (RAAS) with angiotensin converting enzyme inhibitor and angiotensin receptor blockers has been a reasonable strategy for the last 2 decades. There was little else to manage diabetic kidneys apart from RAAS inhibitors, till serendipitous data on a new class of glucose lowering data appeared. Sodium glucose co-transporter 2 (SGLT2) inhibitors have been found to have the added benefit of arresting and reversing kidney disease in patients with diabetes. Randomised trials with SGLT2 blockers have shown substantial reduction in clinical cardiovascular events such as cardiovascular mortality and hospitalisation for heart failure. Now mercifully we find that an SGLT2 blocker can favourably affect kidney disease in patients with diabetes apart from its glucose lowering effect.
More than 26 lakh patients received dialysis or kidney transplantation in 2010. This number will double by 2030. Five to 10 million people are estimated to die from kidney disease worldwide every year.As already mentioned ACE inhibitors and ARB’s prevent adverse kidney outcomes in patients with diabetes and therefore are recommended by all clinical practice guidelines in patients with diabetes with kidney disease or at high risk of developing kidney disease. Crucially end stage kidney disease carries a high risk of mortality, fewer than 50% on dialysis will be alive at the end of 5 years. The risk of death and heart disease is exponentially increased in patients with less severe kidney disease with any incremental lowering of eGFR or increase in albuminuria. Three large randomised trials with SGLT2 inhibitors , EMPA-REG OUTCOME ( empagliflozin), CANVAS Program (Canagliflozin) and DECLARE (dapagliflozin) included patients with type 2 diabetes and known cardiovascular disease (60%), or with multiple cardiovascular risk factors (40%). Each of these trials demonstrated significant reduction in composite kidney disease outcomes (defined as either doubling of serum creatinine or a 40% reduction in eGFR), end stage kidney disease , or death because of kidney disease. But fewer than 17% of patients had a baseline EGFR less than 60 mL/L/ 1.73m2. Thew mean baseline eGFR in all 3 trials was greater than 74 mL/L per 1.73 m2.
But the CREDENCE with canagliflozin studied patients with type 2 diabetes having microalbuminuria and baseline eGFR of 56 Ml/L per 1.73 m2, and showed a 30% relative reduction in composite kidney outcome of end-stage kidney disease (dialysis for at least 30 days, transplantation, or eGFR <15 ml per minute per 1.73 m2 for 30 days), doubling serum creatinine or death from kidney disease or heart disease ( N Engl J Med 2019;380:2295-306). Four thousand four hundred patients with diabetes and established kidney disease received 100 mg of canagliflozin for placebo in a double blind manner in addition to an ACE inhibitor or an ARB. There was also a 20-30% reduction in cardiovascular outcomes. Glycated hemoglobin was reduced more by canagliflozin, as were blood pressure and body weight. Fractures and lower limb amputations were similar in the canagliflozin and placebo groups, but diabetic ketoacidosis was more in the canagliflozin cohort (2.2 vs. 0.2 per 1000 patients years). The mechanism of action most probably is efferent arterioles vasoconstriction that reduces glomerular perfusion and intra-glomerular pressure. There is reduction in eGFR initially but this soon stabilises.
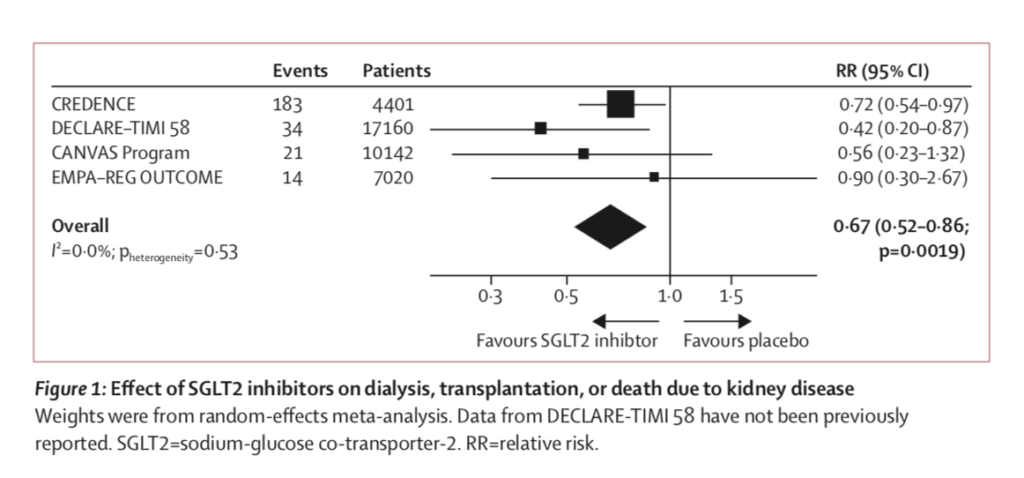
A large meta analysis including 37,723 participants looking specifically at kidney outcomes with an SGLT2 blocker has reported significant reductions in the primary kidney composite outcomes of need for dialysis or transplantation or death due to kidney disease (relative risk 0.67, p=0.0019) ( Lancet Diabetes Endocrinol 2019; published on line September 5,2019).
The robust reduction in kidney outcomes was independent of baseline albuminuria and use of an ACE inhibitor or ARB. Reduction was greater when baseline eGFR ranged between 45 and 60 ml per min per 1.73 m2 ( 45% relative reduction) than when baseline eGFR was between 30 and 45 ml per minute per 1.73 m2 (30% relative reduction). These findings strongly suggest that SGLT2 blockers work better when eGFR is less attenuated. Importantly, acute kidney injury was lowered by 25% (p < 0.0001) in the CREDENCE trial.
In summary the latest meta analysis supports the principle that SGLT2 inhibitors provide protection to the kidney in a broad range of patients with type 2 diabetes; in patients with both preserved and compromised eGFR, independent of their glucose lowering effect. SGLT 2inhibitors reduce risk of dialysis, transplantation, or death due kidney disease in patients with type 2 disease and provide protection against acute kidney injury. SGLT2 inhibitors are available in India.