
More than a decade ago a brilliant American marathoner form the United States collapsed and died 5 and a half miles into a marathon trial run for the Beijing Olympic Games. Ryan Shay was a world class long distance runner whose own Dad was a running coach. When Ryan was only 14 years old it had been noticed that his heart was a bit larger than most children, but this was ignored by everyone including his parents because he excelled in sports. Ryan had run numerous marathons before his death and was therefore presumed to be supremely fit. His death sent tectonic waves across the running world of north America. His legacy endures today with a prestigious annual mile race named after him. I had wondered aloud the on the cause of his death, and wrote so in the Times of India, Delhi edition then. I was afraid that maybe a drug had dome him in. The autopsy report was released more than 4 months after Ryan’s sad death. The report stated that Ryan did indeed have an enlarged heart but with dome scar tissue. It was surmised that viral myocarditis some time in the past accounted for the fibrosis in the young athletes heart. Ryan Shay died when only 28 years old. The normal electrical impulse of the heart is obstructed by fibrosis or scar tissue; it is rendered chaotic resulting in arrhythmia (irregular heart beat) ,which in turn can be fatal. The autopsy report of Ryan Shay concluded that fibrosis due previous viral myocarditis led to sudden cardiac arrest (SCA). There was no trace of hypertrophic cardiomyopathy in Ryan’s case, nor any evidence of a performance enhancer.
Most data on sudden cardiac arrest points out that the leading cause of death in young sportsmen is hypertrophic cardiomyopathy. Hypertrophic cardiomyopathy is a genetic disease (not rare) in which the heart muscle is thickened disproportionately in an erratic manner at the cellular level. The heart muscle cells are not arranged in an orderly fashion under the microscope, there is no brick by brisk pattern of a wall seen in hypertrophic cardiomyopathy. The cells are completely chaotic like an imaginary Van Gogh painting if drunk; this is the microscopic hallmark of hypertrophic cardiomyopathy apart from an obviously thickened heart , which can at times be asymmetric as well. The thickened heart muscle can be recognised on 2 D echocardiography by a reasonably trained doctor, or even a technician. One does not have to wait for a post mortem to confirm obstructive cardiomyopathy. But it should be remembered that elite athletes especially endurance athletes may have enlarged hearts too, accompanied by changes in the their ECG. An astute physician or cardiologist would be required to distinguish physiological heart enlargement from the pathological genetic one.
The question that arises is whether sudden death in a sportsperson can be prevented? Ideally one should be able to preempt the catastrophe of SCA in a young athlete in the apex of his physical prowess. The Italians launched a program of pre competitive screening among athletes and this brought down casualty by almost 90%. But most other nations are wary of a screening program primarily because the incidence of sudden cardiac arrest is very uncommon. Almost rare ,and hence screening would be cost prohibitive. This is endorsed by a recent paper recording incidence of SCA in sportspersons.
The reported incidence of sudden cardiac death in young (< 35 years) varies from 1 to 6 cases per 100,000. This statistic includes death during times of rest also. Incidence of sudden death during competition is as low as 0.5 cases per 100,000 person-year. The latter means that half a person would die suddenly by active participation of 100,000 people in one year. Hence if 100,000 athletes competed for 2 years , there would be one sudden death. The Rescu Epistry provides a prospective registry of all persons who had out-of-hospital cardiac arrest and were treated by an emergency medical team. The researchers report that there were 74 sudden cardiac arrests in 18.5 million person-years over period of 5 years. These deaths occurred during participation in sports. There were 74 sudden cardiac arrests during participation in sports, of these 16 occurred during competitive sports while 58 occurred during non competitive sports (gym or running).The incidence was 0.8 cases per 100,000 athlete-years. Almost 44% managed to survive until they were discharged from hospital. The researchers identified all out of hospital cardiac arrests (deaths and resuscitations) in people aged 12 to 45 years.
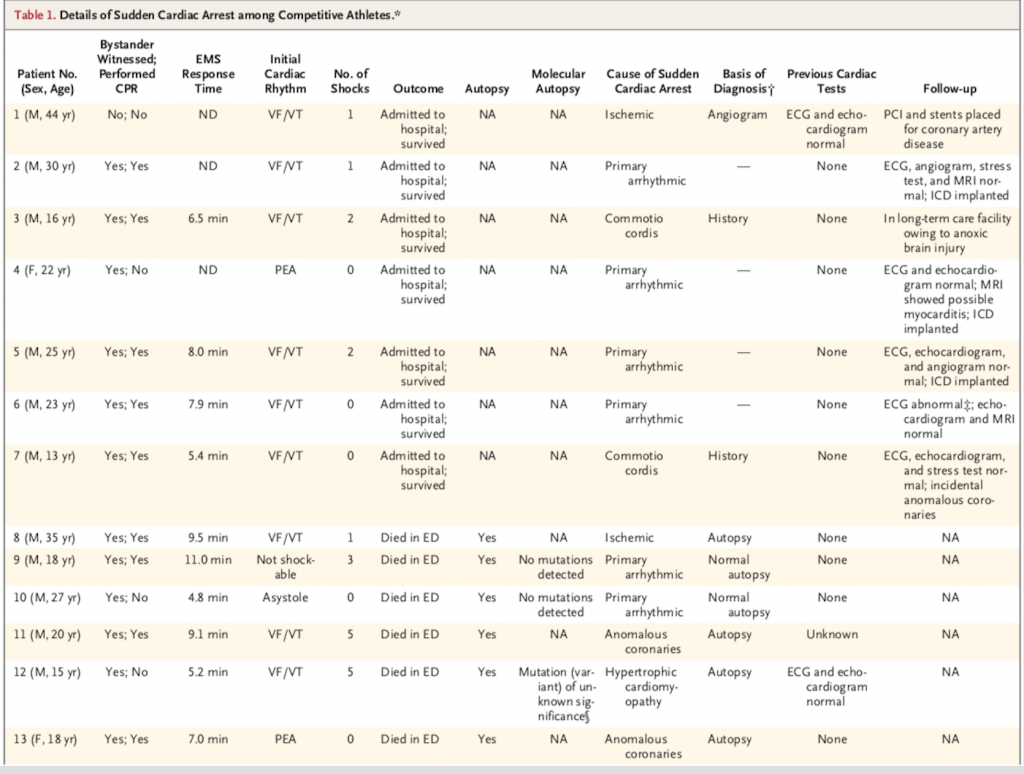
Of the 16 cases of sudden cardiac arrest among competitive athletes, 2 were attributable to hypertrophic cardiomyopathy and none to right ventricular cardiomyopathy. The authors concluded that at least 146,000 athletes would have to be screened to identify one person who would have sudden cardiac arrest during competition. The study underscores the rare incidence of sudden cardiac arrest among athletes as well as the low incidence of structural heart dies that could have been picked up during pre-screening. The rarity of sudden cardiac arrest due to hypertrophic cardiomyopathy or other structural heart disease recorded in the Rescu Epistry suggests that pre-screening for potential heart disease may be an overreach.
The scenario in India is quite different. Let us face it, we are a sedentary nation. Maybe its the heat or the battle for sheer survival. A minuscule of the country’s population is into active sports. We should therefore not follow the American model of avoiding pre-screening. We can afford to pre-screen almost all high level competitive athletes. These should include all athletes participating at the state or the university level. India has both time and the resources to do this. She could start with the oldest and simplest device available to us; the 12 lead electrocardiogram (ECG). The slightest suspicion on an ECG must warrant detailed examination of the sportsperson. The prevalence of pathological T wave changes on the ECG are not more than 2-3%. Athletes with such changes must be scrutinised further.
A French study looked for pathological ECG changes in more than 6000 athletes . They reported 155 athletes with pathological changes. (T wave inverted in almost all precordial leads). Cardiac disease was established in almost half of these people. Hypertrophic cardiomyopathy was the most common disease (80%). Echocardiography identified 54% cases but cardiac MRI picket up another 24 (35%) athletes with hypertrophic cardiomyopathy. Cardiac MRI significantly increased the diagnostic capability of disease identification, particularly in those athletes with apparently normal echocardiographic studies. Also disease may express later on in years, therefore all athletes with abnormal ECG’s but normal echocardiograms or MRI must be evaluated annually. There were 5 athletes considered normal in the French study who expressed disease on fellow up.The decision to permit an athlete to continue competition becomes tricky in the presence of pathological ECG T wave inversion but no evidence of structural heat disease on echo or MRI. In such cases a good family history becomes mandatory with the cautious advice to continue non competitive sporting activity but saddled by an annual check up. All 54 athletes found to have hypertrophic cardiomyopathy (0.85%) were disqualified from participation. The prevalence of hypertrophic cardiomyopathy in the general populations is to the tune of 1 in 500, so certainly not a rare genetic disease.
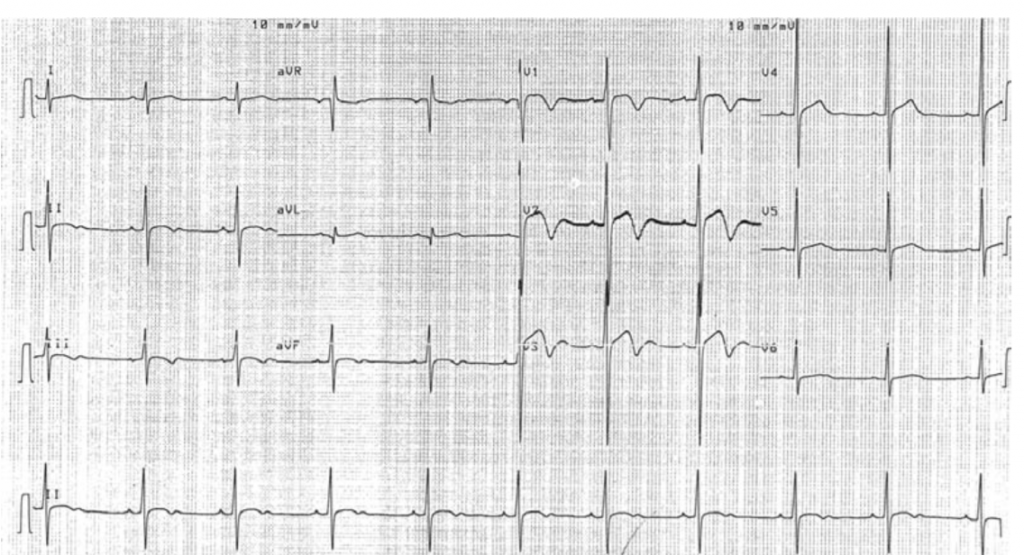
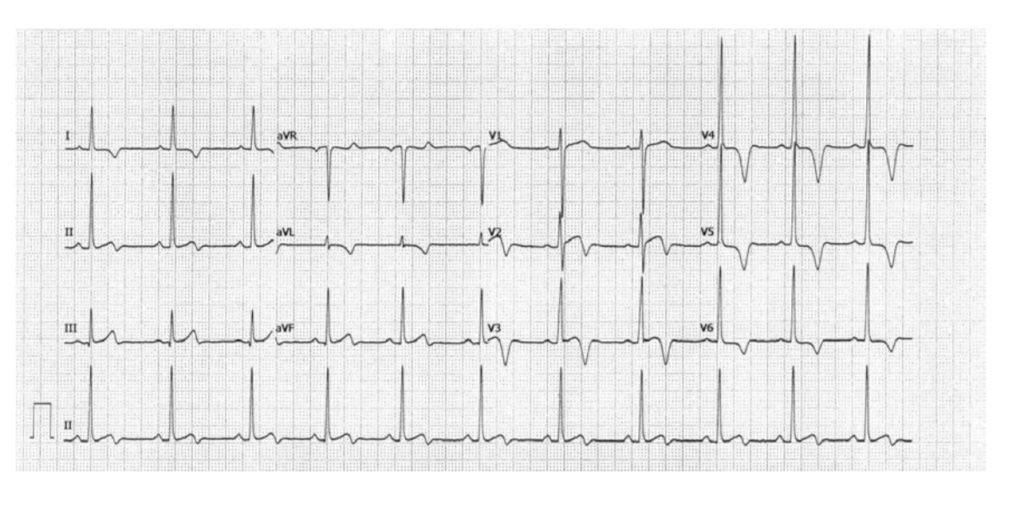
It is universally agreed upon that history taking and physical examination is mandatory. The problem is that most athletes with an underlying heart disease have no symptoms. Also almost 75% of hypertrophic cardiomyopathy patients do not carry a cardiac murmur. But physical screening by a physician is still essential. The addition of an ECG substantially increases the ability to identify potential candidates for sudden cardiac arrest and death. False positives are down to just 2%. Physiological ECG (adaptation to exercise) changes largely consist of T wave inversion in leads AVR, lead 3, and V1to V3 (preceded by coving of ST segment). Pathological T wave inversion is observed in almost all leads. A general physician could do an excellent job in the initial recognition of an altered ECG. In case an alteration is detected a specialist will be needed next for further examination. This will entail trans thoracic echocardiography followed up if possible by cardiac MRI. Payment becomes a problem with cardiac MRI, but this could be subsidised by the state. A correct diagnosis is crucial because death can be averted. The reverse is also true, a false positive diagnosis can be psychological blow to the person concerned apart from financial loss. I really don’t know whether a protocol for pre-screening in young sportspersons is in place in Indian schools and universities.