The occasion was the Annual meeting of the Cardiological Society of India ( CSI ; Delhi , and I had been entrusted with the job of debating that “Aggressive treatment in hypertension had Abundant Evidence.” I had to speak against the motion and was quite convinced that the work cut out for me would not be too much of a bother. I however had not anticipated the turn of events that were to unfold in the hall. To begin with strangely nowadays the Annual CSI does not seem to attract the cardiologists or physicians of Delhi. They would come in droves in the eighties and ninetees One would expect with 3 leading institutions of the country offering a doctor in medicine (DM) degree in cardiology there would be senior residents in cardiology attending the Meeting. Maybe cardiologist in training in Delhi do not consider the annual CSI meeting worthy of providing any additional knowledge to what they already possess. In out times the teaching faculty of G B Pant Hospital, New Delhi insisted that we attend these meetings to fill up on our rather scanty knowledge of cardiology. Similarly residents of the All India Institute of Medical Sciences to were nudged to make sure they got around to attend bits and pieces of the conference, duties permitting. Currently apart from the 3 large teaching hospitals , other institutions in Delhi provide DNB cardiology courses, but I doubt if there was single one of the fellows in attendance.
There were far more empty seats in the auditorium of a swanky 5 star hotel in the heart of Delhi than those that were occupied. Your shoulders do slump a bit with you face an empty hall. The effort put in making a talk can be considerable and especially so when gathering relevant data for a fiery debate. I was quite conscious of the emptiness in the hall as I got up to speak but worse was to come. I have always prepared my slide presentation on “Keynote”, which is an Apple Mac product. I carry it on my iPad, while earlier many years ago I would attend these meetings with my MacBook. The iPad is connected by a VGA adaptor to an HDMI cable that goes on to the projector. I possess a VGA adaptor and all these years the HDMI cable that costs from Rupees four hundred to five hundred only is provided by the projection team hired by the organisers of the meeting.
To my horror I realised when I was standing right there at the podium that the chaps did not have the required cable to connect my iPad with my much laboured presentation. I was at a complete loss of words, I realised there was no way that I could now show my slides. My presentation had been shattered and I could not do d thing about it. What a waste. This was the Annual Delhi Cardiology Meeting without a Rupees five hundred cable. The projection personal and the young woman in charge appeared to have never heard of Apple, or of an iPad.
I was left with no choice but to speak without my slides. A talk in a cardiology meeting is not a trifling matter, it is not a political speech nor one of those supercharged Indian television debates. It obviously became a bit awkward and difficult for me to speak to the audience. But as I said I had no choice. Even as I spoke I raised that it was not easy capturing the attention of the audience; and explaining to them the nuances of my interpretation of data was even more difficult. I had mercifully gone over my talk quite a few times and so knew a lot of it by heart; even the numbers and name of the authors. To me what I wanted to convey was important and I therefore a penning it down now.
Raised blood pressure also termed hypertension is a greatly employed phrase because it is one of the biggest risk factors for heart attack, heart failure, stroke and mortality. Over the years we have known that high blood pressure can play havoc with ones health and life, we have also learnt that by administering anti hypertension pills we can substantially reduce these clinical events stemming from high blood pressure. But what has never been never established was how low we could bring down raised blood pressure to be effective without increasing the risk of adverse effects.
The JNC 7 (Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) in 2003 promulgated that hypertension be defined at 140 mm Hg systolic and 90 mm Hg Diastolic for all ages, while diabetics and patients with kidney disease be treated if their blood pressure exceeded 130/90 mm Hg. The bar was raised to 150/90 in patients aged 60 years or more in 2014. The American Heart Association along with the American College of Cardiology came along with their own set of guidelines at the end of 2017, in which they have lowered the threshold to only 130/80 mm Hg. In one stroke the AHA and ACC have increased the number of “hypertensives “ in the world by millions. Already more than a billion people suffer from raised blood pressure as per the JNC 8 definition. In the United States alone the number of hypertensives will jump from 36% to more than 46%, the figures in African Americans will jump up from 45% to almost 60% or more of the adult population. The prevalence of hypertension by the old definition among people in their thirties in Delhi had been more than 30% almost 2 decades ago. It would to be surprising if 50% or more of the adult population in Delhi would turn out to be hypertensive by the new definition. The broadening and lowering of blood pressure threshold should be examined carefully before subjecting millions of people to antihypertensive pills.
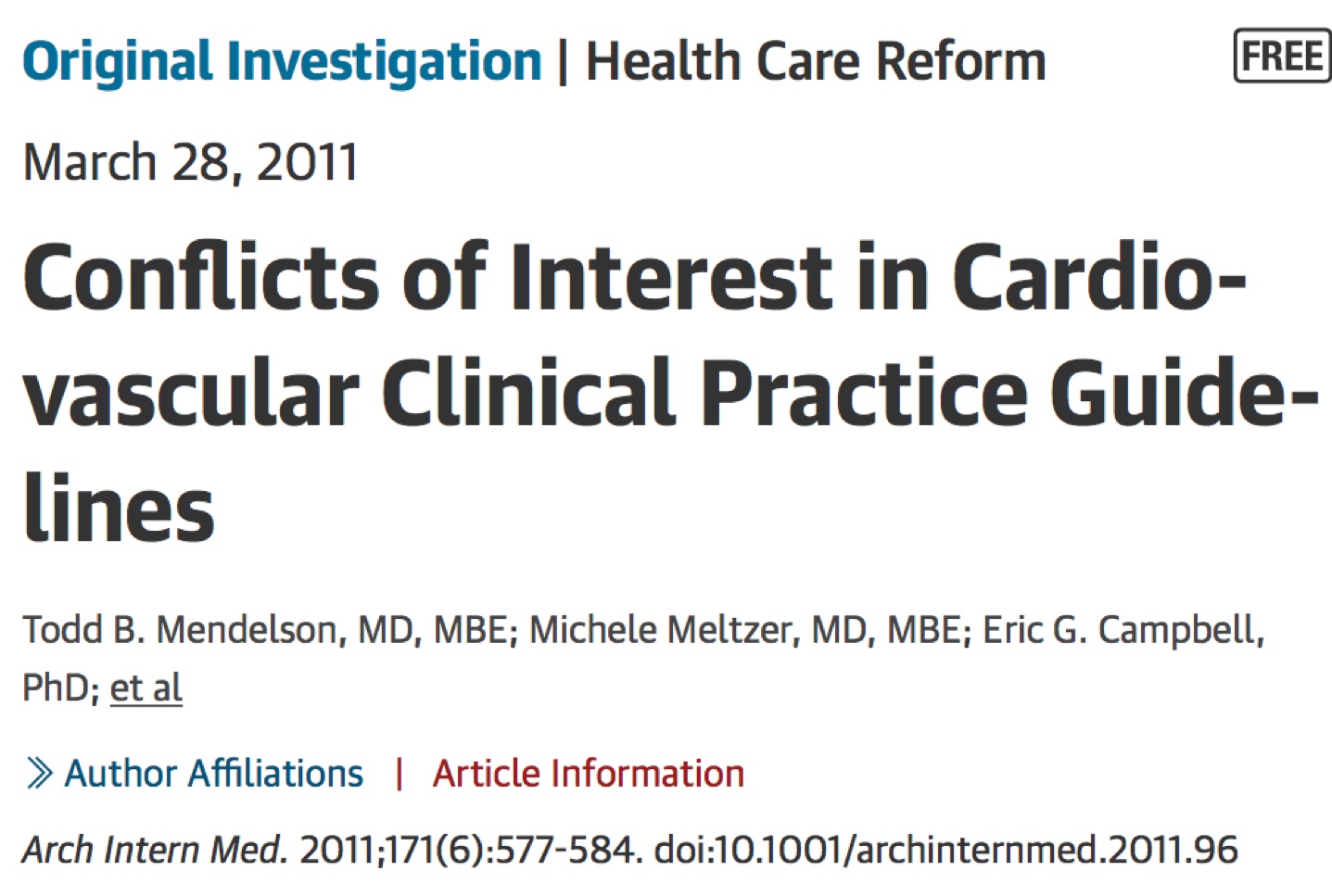
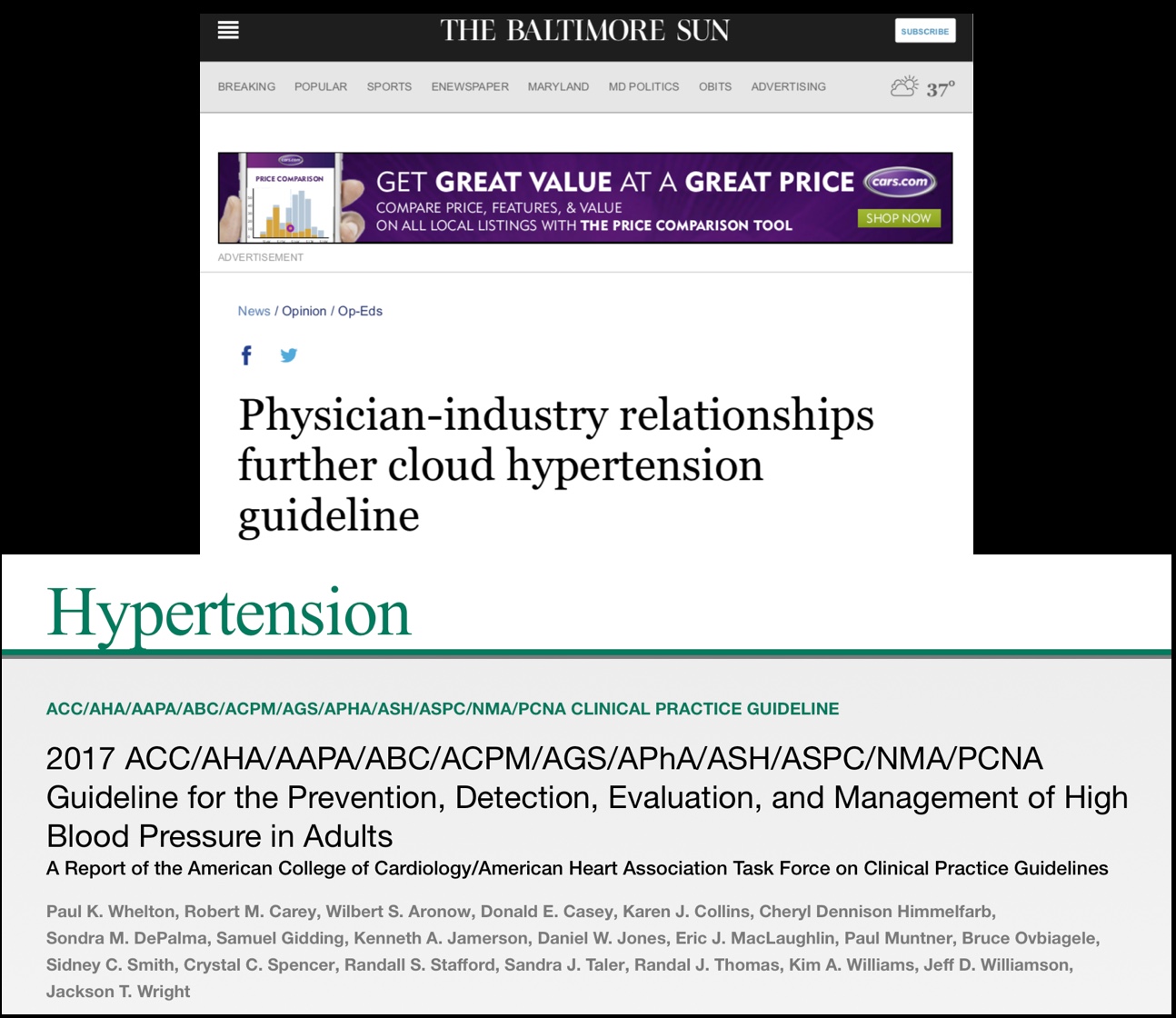
There have been murmurs that 6 of the 16 committee members of the AHA/ACC hypertension committee have fiancée ties to drug companies. It has also been pointed out that 6 members are no strictly speaking blood pressure experts. In 2011 JAMA had come out with a paper that made the startling suggestion that more than 50% of committee members of AHA/ACC of around 17 guidelines had financial ties with pharmaceutical companies. It is obvious that despite best intentions subtle positive feelings for a drug company are bound to creep in. It becomes a matter of concern if financial support is being provided by companies manufacturing blood pressure pills.
The latest AHA/ACC guidelines concede that they have limited evidence in treatment of what they call stage 2 hypertension, or what was previously known as mild hypertension ( blood pressure more than 140/90 and yet they give Class 1 recommendation for treating such people. This is very intriguing because a high quality meta-analysis and review of treatment of mild hypertension done by a Cochrane group failed to show any clinical difference between drug treatment of mild hypertension and placebo. The Cochrane group assessed almost 9000 participants with mild hypertension in 4 randomised trials, the participants were followed for 4-5 years, at the end of which there was no difference in mortality, heart attack, or stroke. In fact an absolute 9% of participants withdrew from their respective trials. The verdict according to the Cochrane group was clear, there was little happiness in treating people with mild hypertension. Cochrane is recognised for providing high quality evidence based data. So now we have a situation where without any clear evidence that anti hypertensive medication work in people with blood pressure of 140-159/90-99, we have the AHA/ACC manadarins recommending in the loudest manner possible that we treat such people. There is total disregard for the manifest collateral damage with such an offensive, moreover the AHA/ACC themselves concede that they say so armed with limited data.
The AHA/ACC guidelines also mandate that secondary prevention is highly recommended (Class 1) in people with diastolic blood pressure more than 80 mm Hg. But once again they concede that the level of evidence is based upon “expert opinion” or EO. The irony is there for all to see. As per the AHA/ACC manadarins it is mandatory that a systolic blood pressure greater than 130 mm Hg be treated (Class 1 recommendation), but this time the level of evidence is A, implying there is at least one one or more high quality randomised study to back the strong recommendation. The American Academy of Family Physicians have however publicly declined to endorse this diktat by the AHA/ACC. The American College of Physicians too are not to excited by the ACC/AHA guidelines.
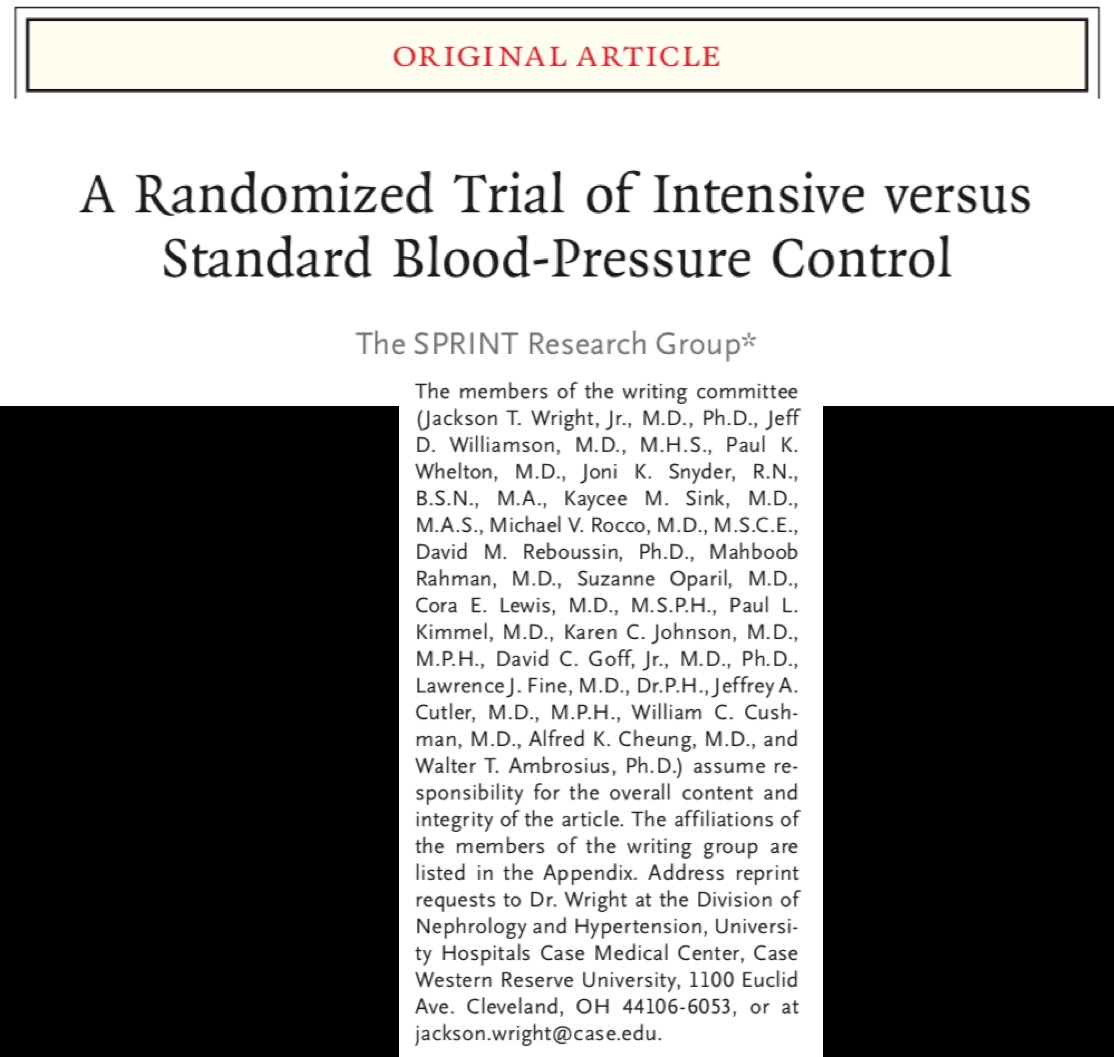
The American Academy of Family Family Physicians are sceptical because of numerous reasons, the most important being that the principal investigator of the “Sprint Trial” is Chairman of the AHA/ACC guideline committee (Paul Whelton) Also 2 more senior investigators of the “Sprint Trial” have been incorporated into the AHA/ACC hypertension guideline committee of 2017 (J.Williamson and J Wright). Is there any wonder that the AHA/ACC hypertension guideline relies almost entirely upon the Sprint Trial . The Sprint Trial randomly assigned almost 9000patents with considerable risk factors to achieve a systolic blood pressure below 120 mm Hg or standard treatment to obtain a blood pressure of 140 mm Hg. The patents had to have at least one risk factor, from latent or clinical cardiovascular disease (but no stroke), compromised kidney function, a Framingham risk score of at least 15$% at 10 years, or age more than 75 years. A diuretic (chlorthalidone) and an ace inhibitor were provided free of cost. Diabetics were excluded from the trial. The trial was aborted after 3.3 years because the safety monitoring committee felt there was clear evidence of efficacy. There were a flurry of supercharged headlines in mainstream media (including the New York Times) about vantages of treating blood pressure to 120 mm Hg systolic or less. The headlines screamed of the relative 25% decrease in clinical events with intensive treatment as opposed to standard treatment, and also of the 27% reduction in mortality. The detailed numbers were however not provided. We had to wait some months before the New England Journal of Medicine published the entire data with an editorial stating they were “proud” to publish the results of the Sprint Trial. An article on a clinical case was also published, in which the proponent for intensive treatment did not hesitate to write that there were no significant differences in adverse events in the two groups of the Sprint Trial.
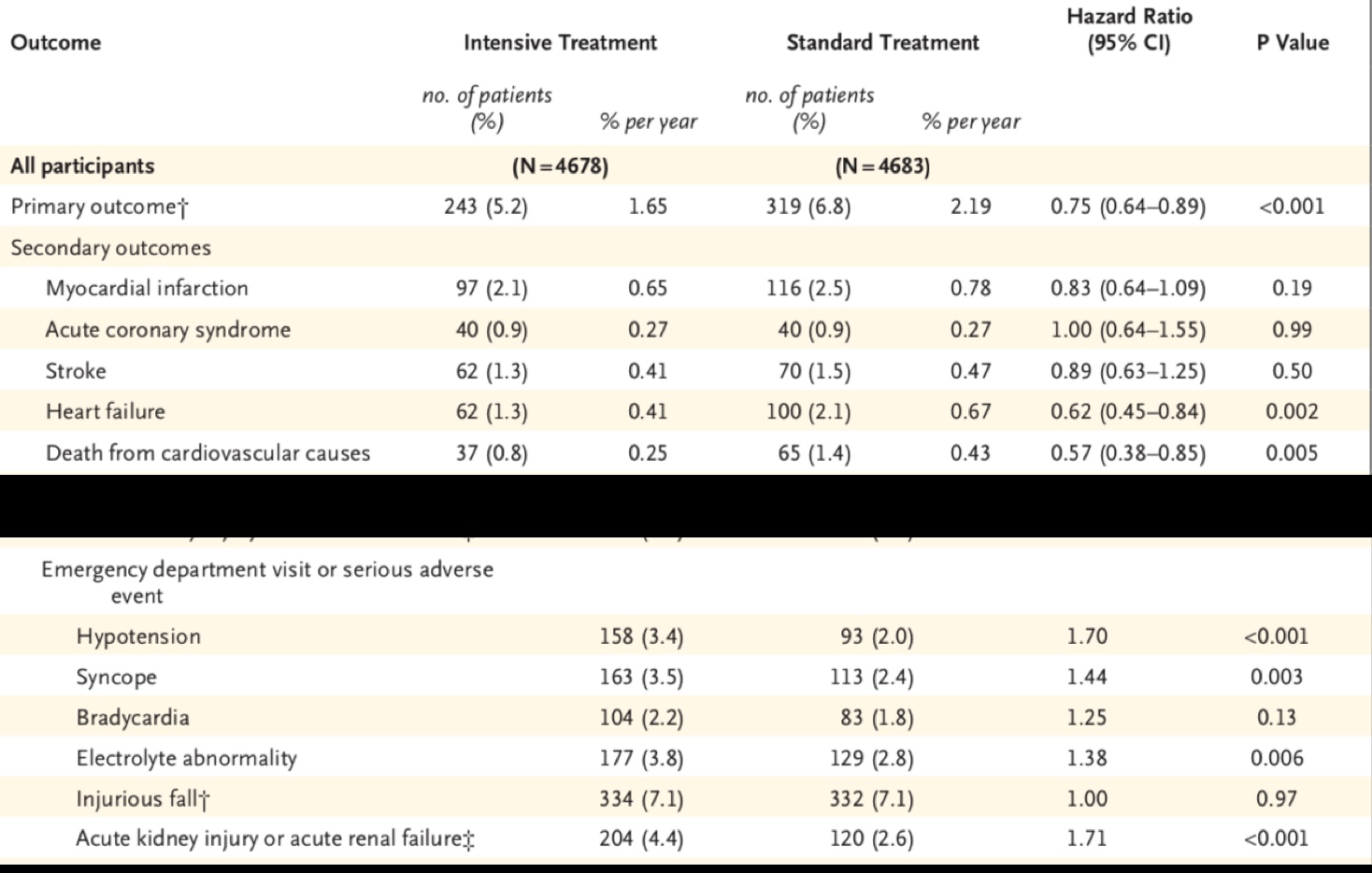
The devil lies in the details. On examining actual clinical outcomes it becomes clear that in the Sprint Trial despite a relative 25% lowering of clinical events by intensive treatment the absolute differences were minuscule.Heart attack were reduced by 0.4% (2.5-2.1%), acute coronary syndrome not at all (0.9% to 0.9%), stroke was lowered by a miserly 0.2%(1.5 to 1.3%), and cardiovascular mortality from 1.4% to 0.8%. Each one of these changes is not significant. Worse, serious adverse effects requiring visit to a hospital emergency were significantly more in the intensively treated group. Hypotension was raised by 70%, syncope by 40%, and acute kidney injury by 70%. Crucially, a subset analysis of participants with base line blood pressure of more than 160 mm Hg and Framingham risk score less than 30%, had significantly greater mortality when blood pressure was lowered below 120 mm Hg.
It is no wonder that when actual data got published there was some turbulence generated. The Prince Trial soon became controversial. Criticism included the fact that almost 90% of patients were on treatment at baseline, the trial was prematurely terminated, clinical benefits were minute, adverse effects outweighed efficacy, measurement of blood pressure was a trifle too complicated, the trial was not blinded, and despite all efforts mean blood pressure in the intensively treated group hovered at 121 mm Hg. The Sprint Trial managed to create considerable doubts about the advantage of lowering blood pressure beneath 120 mm Hg. And yet the AHA/ACC guidelines depend largely on Sprint in their class 1 recommendation to lower systolic blood pressure below 130 mm Hg.
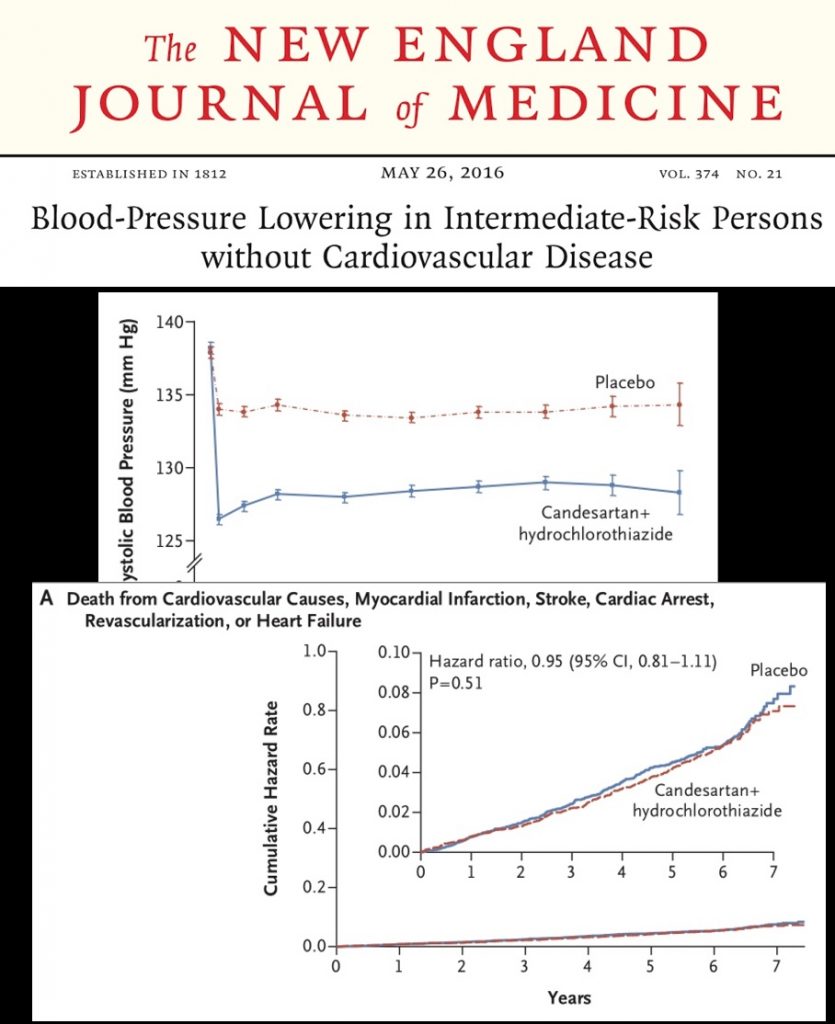
The HOPE 3 trial comparing intensive treatment with candesartan and hydrochorthiazide to standard treatment in 12000 patients of high blood pressure with intermediate risks could not demonstrate improved clinical outcomes. The HOPE 3 trial is the only randomised trial with almost 14% participants of South Asian origin. The ACCORD trial on diabetics too did not show any significant difference in clinical outcomes in patients treated to 120 mmHg as compared to 140 mm Hg over a follow up of 5 years.
A recent meta analysis of 49 trials including more than 70,000 patients with type 2 diabetes demonstrated significantly increased mortality when baseline blood pressure was 140 or less. Reduction in mortality was seen with baseline pressure exceeding 150 mm Hg, and neutral results between 140-150 mm Hg.
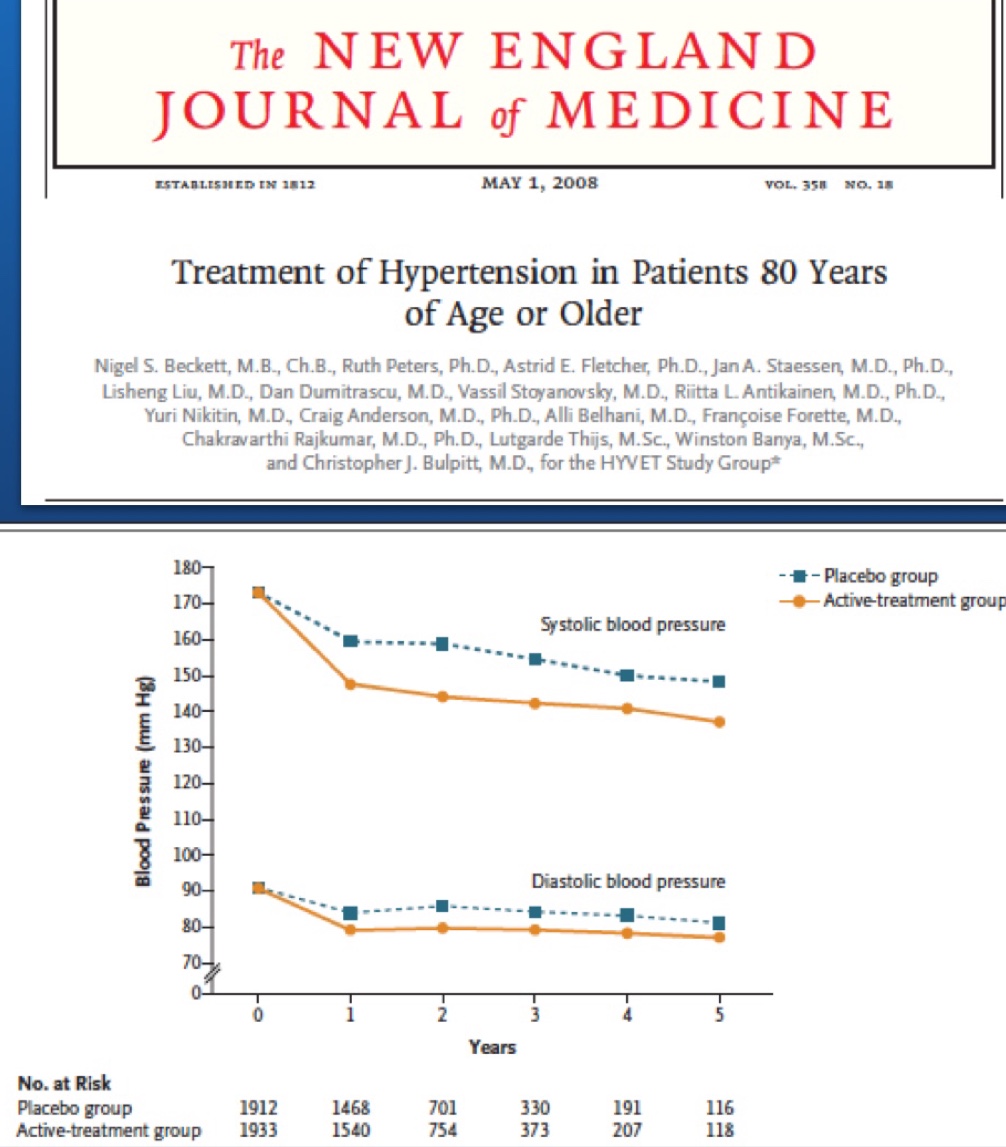
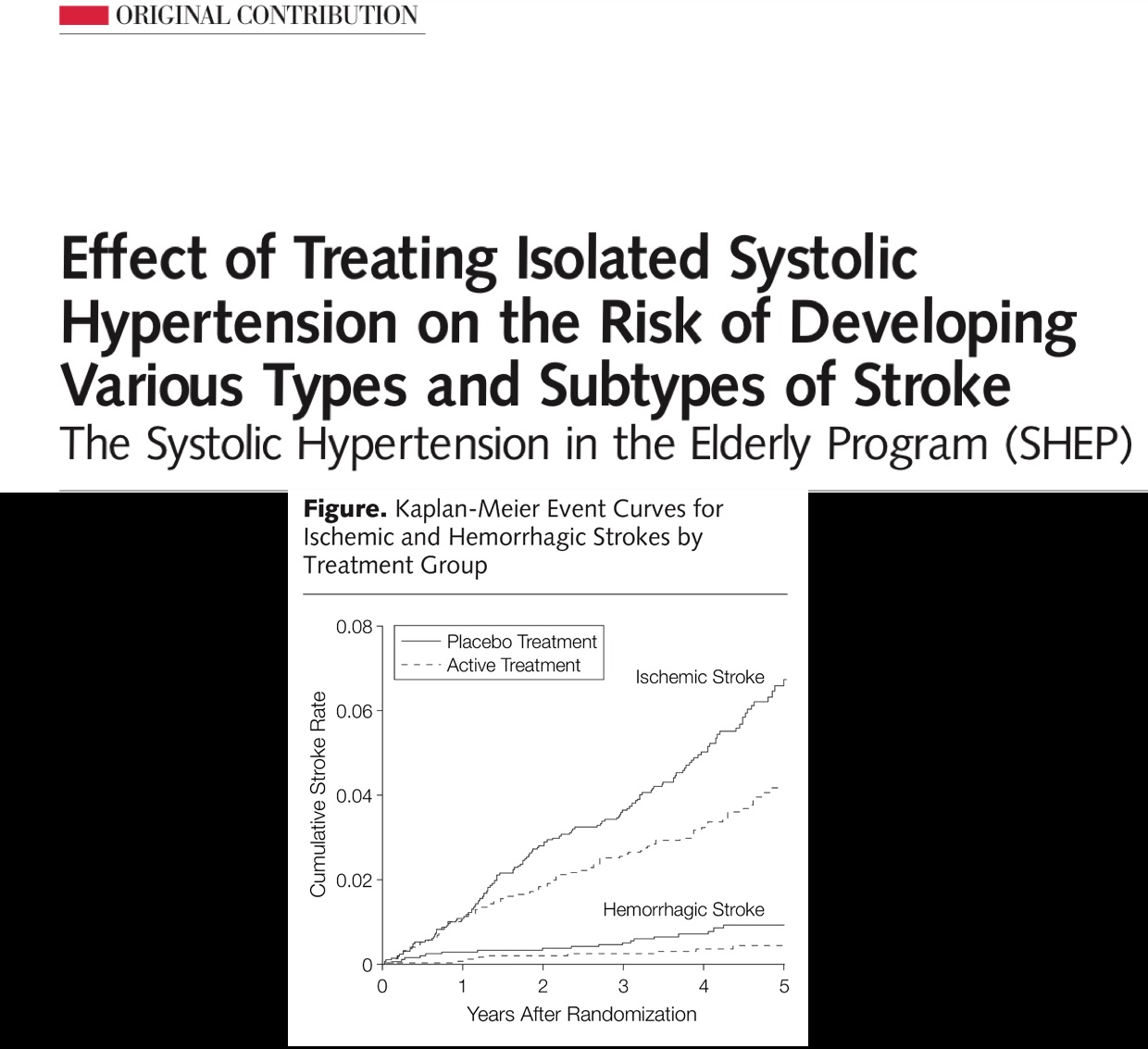
HYVET and SHEP were landmark randomised trials of hypertension ( treatment ) in people over 60 years. Both were randomised trials with almost 4,000 patients each. The mean age in HYVET was 83 years and there was significant reduction in stroke, heart failure, and over all mortality. The point to be highlighted is that these beneficial results were obtained with mean blood pressure a little below 150 mm Hg in the treated group. Similarly there was significant reduction in ischaemic and hemorrhagic stroke in SHEP with blood pressure in the 140’s in the treated group. Patients were
given stepped up treatment in SHEP, chlorthalidone was administered initially followed by atenolol and reserpine if required. Crucially significant cardiovascular outcomes were achieved in both trials with mean blood pressure in the treated group nestled in the 140’s. This is the chief reason why JNC 8 and the American Acedemy of Family Physicians have maintained the threshold as 150/90 mm Hg in people older than 60 years.
Undoubtedly both the American Heart Association and the American College of Cardiology have done a spectacular job in developing Cardiology not only in the US but all over the world. Indian cardiologist rely almost entirely upon clinical guidelines published by AHA/ACC. As do cardiologists in almost all other nations. It would be prudent however to examine the details provided in every guideline. It would be worthwhile checking out the fine print and also the references provided. The entire adult world cannot be branded hypertensive. The planet should not be permitted to be occupied by American Heart Association and the American College of Cardiology. A meta analysis may be better than the sum of its parts, but it can never provide greater scientific integrity than an adequately powered randomised trial.
The American Heart Association along with the American College of Cardiology are thrusting a new definition of hypertension down our throats. Millions of ordinary people will be branded “ hypertensive” and urged to consume pills for the rest of their lives. The Sprint Trial without showing meaningful clinical benefits constitutes the bedrock of their guidelines of 2017. There is bound to be considerable collateral damage if the blitzkrieg is permitted. A 15 minute brisk walk and common sense eating would be as good if not better than life long antihypertensive pills for managing people with blood pressure in the 130/80’s.