One of the commonest life- saving procedures is percutaneous coronary intervention (PCI) invoving percutaneous coronary angioplasty (PTCA) accompanied by insertion of a stent in patients presenting with acute coronary syndrome. The procedure of PCI has been guided all these decades by coronary angiography in which a dye (or contrast) is injected through a catheter (a thin tube) into the coronary artery under X-Ray vision. More than a million such procedures are performed annually in the USA and a similar amount across Europe. Percutaneous coronary intervention has rapidly replaced open-heart surgery in a significant number of patients ; it has further gained popularity with introduction of more powerful anti-platelet agents and development of second generation drug-eluting stents.
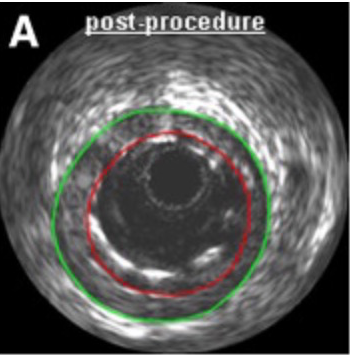
Visual assessment of coronary artery lesions by diagnostic coronary angiography has long been unsatisfactory. Coronary angiography is well known to over estimate or under estimate coronary lesions; also malapposition of a stent or dissection may be missed by coronary angiography alone. This has brought about the employment of intravascular ultrasound imaging (IVUS) in which a tiny transducer is threaded over the angioplasty guide wire and imaging of the concerned vessel be done accurately. Intravascular imaging with IVUS has been found to have much greater sensitivity to detect stent malapposition; which may be then treated with post-dilatation using an angioplasty balloon.
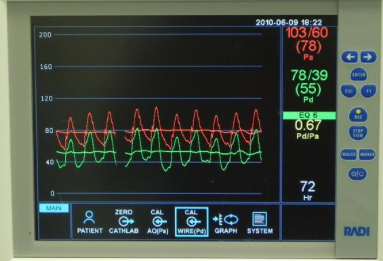
The other imaging modality that has emerged is the pressure wire that is used to detect differences in mean blood pressure distal to a block in the coronary artery as compared to mean aortic pressure. Currently, the general consensuses is that a ratio less than 0.80 between distal mean coronary pressures and mean aortic pressure during maximum hyperemia (by administering intra-venous or intra-coronary adenosine) needs intervention. This is also called fractional flow reserve (FFR). The American Heart Association recommends that FFR should be used for hemodynamic assessment of intermediate coronary (50 %-70%) angiographic lesions in patients with stable angina (indication class IIa). This recommendation is based on randomized trials in which FFR guided PCI compared to angiography guided PCI demonstrated reduced myocardial revascularization with FFR guided PCI (FAME and FAME 2). It is a different matter that clinical outcomes do not differ between PCI and optimal medical therapy in stable angina as shown by the randomized COURAGE trial with a follow up extending of almost 15 years.
Unlike FFR, which provides physiologic or functional effects of a block in the coronary artery, IVUS delivers direct images of the lesion and provides easy measurements of vessel diameter or luminal area. The American Heart Association recommends that IVUS be used to assess intermediate left main coronary artery lesions (class IIa indication).
However it is very important to note that so far no existing randomized data demonstrates reduced cardiac mortality with FFR or IVUS guided PCI as compared to coronary angiography. A recent British audit published in JAMA set out to determine the effect of long term mortality of FFR guided or IVUS guided PCI compared to angiography guided PCI. All patients (41,688) who underwent PCI in London from 2004 to 2011 were included. The primary end point was all cause mortality after a median of 3.3 years.
Fractional flow reserve was used in 6.6% (2,767) patients and IVUS in 4.4% (1,831). At the end of 3.3 years there was no difference in mortality in patients who underwent FFR guided PCI as compared to those had angiography guided PCI (p=0.37). There was however higher adjusted mortality with IVUS guided PCI compared to angiography alone (hazard ratio 1.39, p=0.009). This difference disappeared when propensity score matching was employed (p=0.25). The number of stents inserted were lower with FFR guided PCI as compared to IVUS or angiography guided PCI (1.1 vs.1.3 vs.1.7)(p<0.001). The authors concluded that this large observational study done in London did not show better survival with either FFR or IVUS, but the number of stents deployed were fewer with FFR guided PCI.
Patients receiving a stent were pretreated with clopidogrel (300-600mg) and aspirin (74-300 mg). The use of GPIIb/IIa inhibitors was infrequent. Patients were prescribed statins, life long aspirin, clopidogrel for 1 month (with a bare metal stent) and 12 months (with a drug eluting stent), subsequent to PCI. In total, there were 24,787 patients with stable angina and 16,901 patients with non ST-segment elevation myocardial infarction. Patients with ST-segment elevation myocardial infarction were excluded from this trial.
The FAME study enrolled 1005 stable angina patients with multi-vessel disease. Albeit the composite end point of death, myocardial infarction and repeat revascularization was improved with FFR when intervention was performed in patients with a ratio less than 0.80, no single end point showed significant difference. The FAME 2 trial like wise did not show reduction in mortality with FFR guided PCI but a reduction in need for urgent revascularization in the FFR group of ratio less than 0.80. The British audit including more than 41,000 patients too failed to show improved survival with either FFR or IVUS guided PCI. There may be a stent sparing effect with FFR but there is no mortality benefit; at least not shown in any study so far.
FFR and IVUS are very different procedures; IVUS may be useful in individual cases by defining equivocal lesions, help in stent sizing, and pick up post stenting complications. Intravascular ultrasound apart form OCT , is the only technology available to identify edge dissection and malapposition of stents.
Small randomized trials have not shown any mortality benefit with IVUS.A large trial named ‘Angiography Versus Intravascular Ultrasound Directed stent placement trial’ (including 800) despite showing insignificantly reduced target lesion revascularization with IVUS (8.1% vs. 12%, p=0.08), did not record difference in mortality. The IVUS group had larger stent lumen diameters due to more frequent post-dilatation with a balloon.
The ADEPT-DES Study has been the largest study with IVUS guided PCI included 8583 patients at 11 international centers. The study yet again did not show any reduction in mortality; albeit it did demonstrate lower rates of stent thrombosis and myocardial infarction with IVUS guided PCI wwith insertion of drug eluting stents. The difference though statistically significant was nothing to write home about, when assessed clinically. Stent thrombosis slipped to 0.6% from 1.0 % with IVUS while myocardial infarction dropped from 3.7% to 2.5%. The absolute figures are less than modest. One hundred patients will need to be subjected to IVUS guided PCI to prevent one myocardial infarction and more than 200 patients to prevent a stent thrombosis.
There is as of now no rush to purchase an IVUS machine against the back drop of the city of London audit ( where IVUS was used in a mere 4% of patients undergoing PCI) showing no reduction in mortality , and no randomized trial so far demonstrating a survival advantage.