A significant amount of information was gathered by testing people for antibodies against the new coronavirus in China, Singapore and South Korea. The presence of antibodies against the virus indicates that the person has been infected and more over is now immune to repeat infection. Immunity top measles and mumps lasts a lifetime, whereas tetanus antibodies are present for a decade or so; thats the reason one needs another tetanus shot after 10 years. The first responders to the viral infection will be IgG (immunoglobulins G) that prepares the body for a counterattack against the invading virus. Next IgG (immunoglobulin G) come into play, they directly attack the infecting virus. The quantum of antibodies varies from person to person; some may achieve a large number of antibodies while others may produce a less robust response. Immunity to the coronaviruses producing the common cold or seasonal flu last a couple of years, and hence yearly vaccination shots against them; also the virus mutates, which means it changes its form to such an extent that the immune system fails to recognise it. And therefore the efficacy of the regular flu shot ranges from 40% to 60% only. Experiments done on monkeys suggest that immunity against the new coronavirus causing the Covid-19 pandemic does develop following infection. Antibodies against the 2002 SARS virus have lasted for a decade, and according to some immunity of some sort is present till 17 years.. Crucially antibodies formed by natural infection last longer than vaccines.
Testing for antibodies is called serological testing. The serological test identifies a person who has been infected with the Covid-19 virus but is NOT used to diagnose active infection. The antibodies can be detected as early as 3-4 days once symptoms develop and should stay for at least a few months if not longer. There is no data on duration of immunity against Covid-19 for the simple reason it is brand new evolving disease. Extensive serological testing have been done already in assign countries that has added to epidemiological data on the new Coronavirus. Germany has plans of testing hundreds of thousands people to ascertain the quantum of those infected. The state of New York has approved serological testing. Crucially detection of antibodies will provide a better picture of all those infected-symptomatic, middle symptomatic or without any perceived symptoms. A significant number of people will have to be serological tested, lets say around 10 lacks. This should not be too arduous because the test is substantially cheaper than the RT-PCR, and also gives results within minutes. PCR can take as long as 8-10 hours, while immune assay tests ( also used for diagnosis of virus presence not for antibodies) also give a result in a few minutes. The serological test uses blood while RT-PCR testing is done from swabs collected from the nose, mouth or lung secretions, and even from the rectum. But making the kits is not simple. Sections of the protein of the new coronavirus have to be produced in the laboratory to be used in an immune assay that detects whether antibodies are present. Expressing the protein in the right structure can be difficult. Which is the best protein to elicit antibody production? Most scientists agree the protein in the spikes of the virus are the best. The other protein is the nucleocapsid protein. It will be important to distinguish antibodies against common cold coronaviruses.
The serological test by identifying previously infected (symptomatic or asymptomatic) can be the best tool to decide on when and how to loosen a lockdown. The simple logic is that with serologic testing we can separate those who were infected earlier and now have the immunity to fight fresh infection, from those who were not infected and hence still vulnerable.All health personnel should be ideally tested to allow those with immunity to go back into the front lines. Similarly other vital components of the social fabric such as police, fire men, train drivers etc can resume work. The decision to reopen society, begin schools or colleges and get business back on track will depend upon knowledge of rate of infection and prevalence of immunity. Serological tests should not be used in symptomatic people because they would not have had the time to initiate an adequate response. Also clinicians understand that no test is 100% reliable, there could be both false positives and also false negatives. But this is all that we have in the given circumstances; there is absolutely no data from the US for the CDC to suggest an advisory. Most experts opine that immunity to the new coronavirus may be a couple of years.
However serological testing lakhs of people, albeit necessary will be a logistical and administrative challenge. The tests will have to be reliable and regulatory agencies will need to fast track clearance. But India can easily muster both muscle and cash for mass testing. The data acquired can become a model for other countries to help them implement their future strategies. Every country reeling under this pandemic is wondering when and how to unlock. Unlock we must, the loosening will have to be guarded and gradual. The decision will also depend upon areas reckoned as hot spots. Ten million people becoming jobless is less than a month in the US is most worrying. Serological testing will not be a panacea or some magic formula, it can determine the extent of the problem, it by itself will not stop viral transmission. The public has to follow the protocol of multiple hand washing, physical distancing, and sneezing ettiequte to combat the new corona virus.
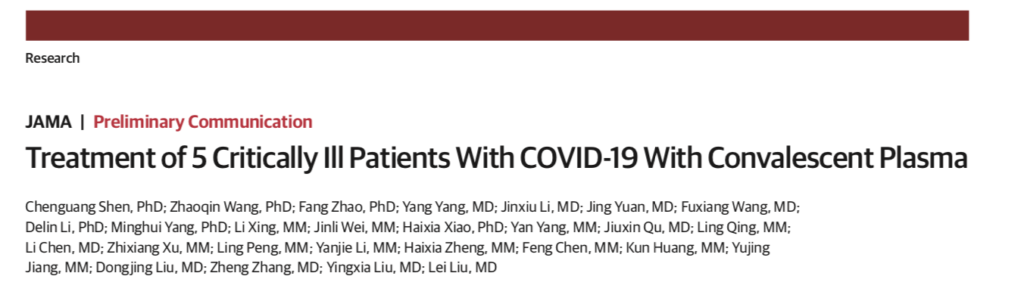
Apart from giving some idea of the rate of infection in the community, and selecting people who can go back to work, the serological test can identify prospective donors. The concept of plasma donation by people who have a robust antibody response to very sick people has been done before. Plasma is what you are left with after separating the various cells in blood. Plasma contains antibodies and coagulant factors. Thus plasma has been administered in extremely ill patients with Hantaan and June virus (both produce hemorrhagic fevers), and also ebola. There are anecdotal reports from China that have successfully used plasma from previously infected people in severely sick patients of Covid 19. Recently a paper that included 5 severely sick patients treated with plasma was published in the Journal of the American Medical association. All 5 patients (2 women) were on ventilator support, 2 had fungal or bacterial pneumonia , and one patient needed extracorporeal membrane oxygenation (ECMO). All 5 patients had high viral load despite anti viral treatment.The researchers ensured that adequate IgG and IgM antibodies were present in the plasma, the antibodies were also checked for antiviral activity prior to administration. There was significant recovery in all patients, fever came down and ventilators could be disconnected. Body temperature normalised in 3 days in 4 patients while viral loads became negative ion 12 days. After 9 days of plasma transfusion 4 patients did not require a ventilator.Three patients have been discharged while 2 continue to be in hospital in stable condition. The authors conclude that plasma from previously infected people containing neutralising antibodies improved the clinical condition of 5 critically ill patients. They also correctly state further studies are needed to validate their findings. This is at best an exploratory pilot study. There was no control group that did not receive anybody loaded plasma. Hence it is not possible to say with certainty that the plasma administered was the magic bullet. It may be possible that the 5 patients recovered because of underlying anti viral and steroid treatment. The convalescent plasma was given upto 3 weeks into hospital admission, so we really do not know of the optimal timing with this intervention in patients infected with the new coronavirus. And most importantly the researchers acknowledge based on their data no conclusion can be drawn on reducing mortality by this treatment.
A study in 2004, on convalescent plasma in the treatment of 80 of 339 suspected SARS patients reported more patients were discharged on day 22 (58%) when convalescent plasma was administered before 14 days as compared to those given after 14 days (16%). Convalescent plasma was obtained from patients who had recovered from SARS.The plasma was given on an average 14 days following onset of symptoms because viral load peaks in the first week. The clinical deterioration that develops after a fortnight is due to inflammatory or hyperimmune response directed at lung tissue. There were no adverts effects because of plasma administration. Mortality in the 80 treated patients with convalescent serum was 12.5% while overall mortality in SARS patients in Hong Kong during that time was 17%. This study also was not randomised so definitive statements on plasma administration in severe patients could not be made; SARS was to soon disappear, so no large trial could be conducted.
But with Covid-19 it may be possible to conduct a randomised trial with convalescent plasma in patients infected with the new coronavirus. The pilot study published in JAMA, and previous research on other viral diseases suggest there may be clinical benefit with convalescent plasma. This needs to be confirmed. Serological testing should be done ,in the meantime, to understand better the infection rate of the new corona virus and to identify health personnel who could go back for frontline work in hospitals. The ICMR has pulled down its earlier advisory on use of serology in hotspots across India ( there are 20 of them). Kerala as per reports has begun using serological tests, while Haryana and Maharashtra are keen to begin. Around 8000 tests (PCR) were conducted today in India, the number of positive cases have risen to 2301, with 56 deaths. There are signals that domestic air and rail bookings may resume from 15th April in India, but they seem to be based more on empirical observation instead of hard scientific data.
The rest of the world there is scrambling to get serological kits by the millions, in order to pick out people who have developed immunity and can resume work. It is mandatory ,as explained earlier, that health workers be checked first to keep health systems up and running, and also that the rest of the population gets back to work. The ICMR has put up a skimpy advisory on antibody testing and also the names of the 6 non FDA/CE approved companies. Britain has ordered more than 17 million home kits knowing very well that the sensitivity in mild cases may be as low as only 50%, this rises to 90% in hospitalised patients. But the fact remains that it is imperative that we begin a serological program with greater zeal to define the prevalence of both disease ,and people with immunity to the SARS -CoV-2 virus. I cannot over emphasise how important it is to test for antibodies in the health workers ; those treating patients in intensive care units are well and truly in the front lines of one of the most unchartered diseases ever. Also, personal protection equipment of the highest standards, is mandatory for health workers confronting this virus on the front line.