Thoracic aortic aneurysm (TAA) is associated with the extreme complication of acute aortic dissection (AOD). People with genetically associated TAA are at greater risk of AOD due to structural alterations in their aorta. Marfan Syndrome (MFS), bicuspid aortic valve (BAV), Ehlers-Danlos syndrome, Loeys-Dietz syndrome, Turner syndrome, and familial TAA are the usual causes of genetic TAA, and of these MFS and BAV are the commonest.
The GenTAC (National Registry of Geneticaly Triggered Thoracic Aortic Aneurysms and Cardiovascular Conditions), a prospective multicenter registry of genetically associated TAA has recently published a paper with the aim of establishing relative risk for AOD in relation to TAA etiology, and to determine association between pre-dissection aortic size and subsequent AOD. The research included patients who had undergone prophylactic TAA surgery.
Aortic imaging was performed by echocardiography, computed tomography (CT) and magnetic resonance imaging (MRI). The study included almost 2000 patients, with patients having BAV being the predominant group (39%). The next commonest group of patients had MFS (22%). Acute aortic dissection occurred in 31 patients (1.6%) in a follow up of 3.6 years. Aortic dissection occurred most commonly in MFS (61%). After 3 years of follow up incidence of AOD was significantly in patients with MFS compared with participants with BAV and the remainder of the registry (GenTAC) population. The incidence of AOD was 6 fold higher in patients with MFS (4.5%) as compared to BAV (0.3%, log-rank p <0.001) and also versus remainder of the population (0.7%, p <0.001).
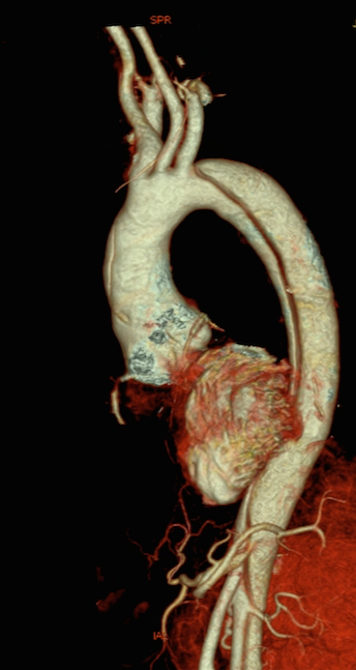
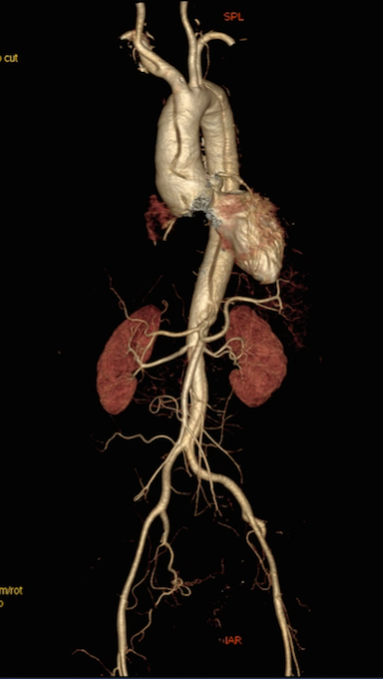
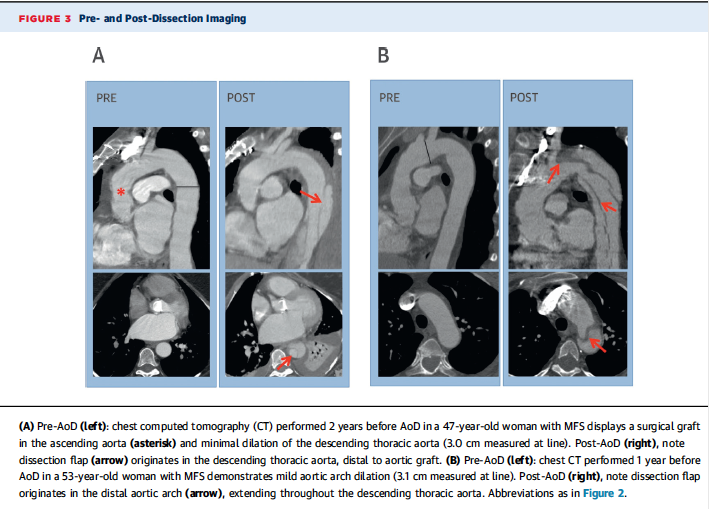
A little more than half (52%) underwent aortic graft implantation before AOD. The grafts were employed in the aortic root or the ascending aorta. In patients with pre-existing aortic grafts, AOD occurred usually distal to the grafted segments (14 of 16 patients;88%).
Echocardiography was the most common imaging technique used in the GenTAC registry. In patients with previous grafts 93% of dissections were of type B (originating in the descending thoracic aorta). But AOD were type A (originating in aortic rot or ascending aorta) in 50% in patients without a previous aortic graft.
The distal aortic size was larger in patients with previous aortic grafts, while the ascending aortic size was similar. In patients without previous aortic surgery the aortic root size was larger in patients with AOD, while distal aortic segments (descending thoracic and abdominal aorta) were of similar size.
Surprisingly, only 11% of patients with type A aortic dissection had an aortic diameter >5.5 cm (root or ascending aorta). In patients with type B aortic dissection, only 14% (3 of 22) had a pre-dissection image of aortic diameter >5.5 cm. It is clear that patients with genetically associated TAA remain at risk for AOD and there is need for new methods to predict which patient is susceptible for future AOD. Conventional imaging in the GenTAC registry has demonstrated that the majority of patients with AOD have aorta diameter within the 5.5% ceiling prescribed by cardiac societies. We may have to search for genetic mutations or a specific biomarker that predicts this devastating complication.
In clinical practice about two thirds of AOD are typically type A and one-third are type B. In the GenTAC study almost one-third of patients had previous aortic surgery and hence type A dissection were relatively few. There were 9 type AOD and 22 type B AOD. The fact that MFS patients had far greater AOD suggests that the pathogenesis and also management should differ from patients with BAV. Fifteen of 22 type B AOD occurred in MFS, but none in BAV patients.
Aortic aneurysms have diverse etiologies and involve multiple segments of the aorta (the aortic root, ascending thoracic aorta, arch of aorta, descending thoracic aorta or the thoraco-abdominal aorta). Thresholds for aortic repair remain uncertain as also medical management of a TAA. The 2010 ACC/AHA Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease decided to lower the threshold to 5 cm from 5.5 cm in patients with BAV. A large study involving 416 patients with BAV revealed, however, that the annual incidence of AOD was 0.4% and that the average diameter of aorta at dissection was in fact larger than in patients with tricuspid valve (66 mm vs. 56 mm, p= 0.0001). The study went against the rule that patients with BAV were more vulnerable. The ACC/AHA Guideline Committee restored the threshold back to 5.5 cm.
It has been reported that in patients with MFS, previous proximal aortic repair was in itself a risk factor for late type B AOD. It is moreover difficult to predict AOD in a patient with TAA. In the IRAD (International Registry of Acute Aortic Dissection) study, almost 60% patients developing type A dissection had proximal aortic diameter of <5.5 cm, while 40% had a diameter <5 cm.
In IRAD, 82% of patients with type B aortic dissection presented with descending aortic diameters < 5.5 cm threshold for aortic repair, and 21% presented with diameters less than 3.5 cm. In the GenTAC study patients presenting with type B aortic dissection had an average descending aortic diameter of only approximately 3.3 cm. It is crucial therefore that we come up with markers that predict AOD more predictably. Aortic diameter measurements by themselves may be inadequate to predict an AOD in MFS patients. A recent Hungarian study reported that raised serum levels of transforming growth factor-B (TGF-B) measured by ELISA, and upregulation of matrix-metalloproteinase 3(MMP-3) gene in patients with MFS who presented with acute aortic dissection. Most patients with MFS have mutation in the fibrillin-1 (FBN1) gene. The aortic wall becomes inelastic and vulnerable to tear with rise in blood pressure. More studies are needed to confirm the role of these molecular biomarkers.