The Future Revascularization Evaluation in Patients with Diabetes Mellitus :Optimal Management of Multivessel Disease (FREEDOM) was the largest randomized trial studying the impact of percutaneous intervention (PCI) with drug eluting stents (DES) versus CABG in patients of diabetes mellitus with multivessel disease. Nineteen hundred diabetic patients (mean age 63 years) were enrolled in 140 international centers; 83% had 3-vessel disease and 71% were men. The DES group received sirolimus or paclitaxel eluting stents, which are now considered first generation DES. Median follow up was 3.8 years. The primary outcome (death from any cause, nonfatal myocardial infarction (MI) or nonfatal stroke) was significantly more common in the PCI patients (27% vs. 19%; p=0.005); driven largely by rates of myocardial infarction (p<0.001) and death from any cause (p=0.049). The CABG group had both lower mortality (6% vs. 13%) and MI (11% vs.16%). Strokes were however more common with CABG (5.2% vs.2.4%; p=0.03). The authors concluded that CABG was superior to PCI in diabetic patients in that it significantly reduced death and MI (1).
The average glycated hemoglobin was 7.8%, left ventricle ejection fraction (LVEF) was 65% in 97% of patients, the mean SYNTAX score was 26 (35% had SYNTAX score <22, 46% had a score between 23-32, and 19% had >33), the number of lesions were about 5.6 while lesions stented were 3.5, and number of grafts were 2.9 of which 95% were left internal mammary arterial grafts.
The editorialist acknowledging that he was neither an interventional cardiologist or a cardiac surgeon (and therefore unbiased); voted in favor of CABG, despite mentioning that stent technology continued to evolve (2). Current European and US guidelines, depending heavily on FREEDOM data, rate CABG as class 1 indication in diabetics with MVD compared to PCI.
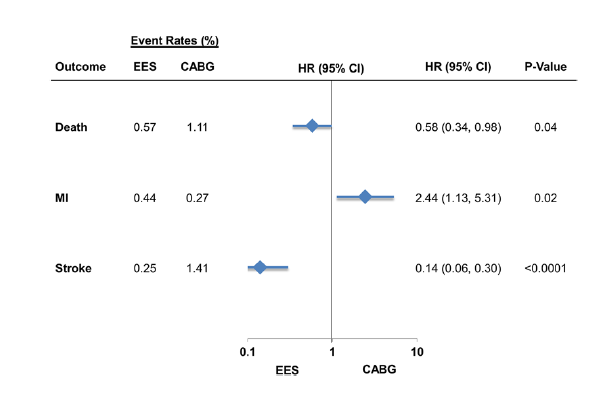
The latest study (3) including patients from the New York State registries has compared CABG with PCI in patients with diabetes and multivessel coronary artery disease employing only the second generation everolimus eluting stent (EES) in the PCI group. The study ,albeit not randomized, has propensity score matched 8,096 of 16,089 patients of diabetes and MVD, to PCI and CABG. At 30 days, PCI with EES significantly reduced all cause mortality by 42% (p=0.04) and stroke by 86% (p<0.0001); but with greater risk of MI (HR2.44; p=0.02).
At long term risk of death was similar between EES and CABG 910.5% vs. 10.23%; p=0.16), lesser stroke (2.9% vs. 3.9%; p=0.04) but higher MI and repeat revascularization. Interestingly greater risk of MI was not seen in patients who underwent complete revascularization; it was also not seen in patients with 2-vessel disease .The study included patients with average age of 65 years; 70% patients had LVEF >50%; 68% were males; and about half of patients had 3-vessel disease.
Patients with diabetes have a greater burden of atherosclerosis and plaques; moreover atherosclerosis progresses more rapidly and can be more diffused as compared with non-diabetics. Patients with diabetes are more prone to develop in-stent restenosis and stent thrombosis, while such patients undergoing CABG are more likely to suffer from deep sternal wound infections, renal failure and worse long term outcomes (4).
The SYNTAX trial too in a sub group analysis of diabetic patients with MVD, reported lower death (13% vs. 19.5%; p=0.065) and MI rates (5.4% vs. 9.0%; p=0.20) at 5 years follow up (5). A meta-analysis of 8 trials published the same year showed reduced long term mortality with CABG compared with bare metal stents or first generation DES (6). The meta-analysis however did not include a single study deploying second generation DES.
One reasonable explanation for the better results with EES may be their thinner struts (81 um vs. 130-140 um) and thinner plus more biocompatible polymer (7.8 vs. 13.7-17.8 um) resulting in lesser inflammation and thrombogenesis accompanied by more rapid re-endothelialization compared with earlier generation DES. The largest data in patients with diabetes involving 22,844 patient years of follow-up from 42 randomized trials had observed that EES was most effective (defined as lowest rate of restenosis) and safest (defined as lowest rate of stent thrombosis) when compared with all FDA approved DES and bare metal stents (7).
Percutaneous coronary intervention with second-generation stents in diabetic patients with MVD most certainly demands a second look and not to mention, adequately powered randomized trials comparing PCI with CABG. In the mean time, PCI with an EES can be considered a viable option in less complex MVD (SYNTAX score less than 22 and possibly even more).
REFERENCES
- Farkouh ME, Domanski M, Sleeper LA, et al. FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012; 367:2375-2384.
- Hlatky M A. Compelling evidence for coronary-bypass surgery in patients with diabetes. N Engl J Med 2012; 367:2437-2438.
- Bangalore S, Guo Y, Samadashvili Z, et al. Everolimus eluting stents versus coronary artery bypass surgery for patients with diabetes and multivessel disease. Circ Cardiovasc Interv 2015; 8:e002626.
- Thourani V H, Weintraub WS, Stein B, et al. Influence of diabetes mellitus on early and late outcome after coronary artery bypass grafting. Ann Thoracic Surg. 1999; 67:1045-1052.
- Kappetein AP, Head SJ, Morice M-C, et al. Treatment of complex artery disease in patients with diabetes: 5-year results comparing outcomes of bypass surgery and percutaneous coronary intervention in the SYNTAX trial. Eur J Cardiothorac Surg . 2013; 43 ; 1006-1013.
- Verma S,Farkouh ME, Yanagawa B, et al. Comparison of coronary artery bypass surgery and percutaneous coronary intervention in patients with diabetes: a meta-analysis of randomized controlled trials. Lancet Diabetes Endocrinol. 2013;1:317-328.
7. Bangalore S, Kumar S, Fusaro M, et al. Outcomes with various drug eluting or bare metal stents in patients with diabetes mellitus: mixed treatment comparison analysis of 22,844 patient years follow-up from randomized trials. BMJ. 2012; 345:e 5170.