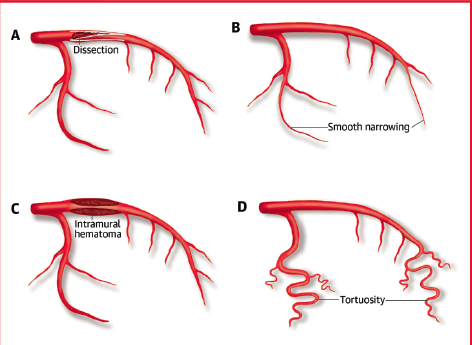
Fibromuscular dysplasia (FMD) is a non-inflammatory disease that manifests as stenosis, dissection, aneurysm, beading or tortuosity. The disease affects mainly women between 30 and 60 years but can affect both sexes and all ages. A rough estimate of prevalence has been estimated from kidneys donated for renal transplant. It was first described in 1938 in a 5- year old boy with hypertension due to unilateral renal artery involvement. It took another 30 years to realize that arteries other than renal could also be involved. In 1964, coeliac, superior mesenteric, splenic and external iliac arteries were found to be involved with FMD.
Now a US Registry including more than 900 patients provides important data regarding clinical implications of the disease.
As per the registry, dissection occurred in 25%, and aneurysms occurred in 20% of patients. Disscetion most commonly occurred in the renal, external cervical and coronary arteries.
The extra cranial carotid, renal and intracranial carotid arteries were the most common sites of aneurysm.
FMD patients with dissection were younger at presentation (48 vs. 54 years of age) and suffered from more neurological and ischemic events than those without dissection.
The most common histological type of FMD is a medial fibroplasia, which results in an artery with a “string of beads” appearance due to areas of fibrotic stenosis followed by post stenotic dilatation. The string of beads appearance is now called focal FMD, while focal FMD is a single area of tubular stenosis due to intimal hyperplasia. The prevalence is derived to be 4% from asymptomatic kidney donors. The prevalence may be higher in patients with resistant hypertension. In the US registry 94% of patients are women.
Extra-cranial and vertebral artery involvements are associated with migraine type headache, tinnitus, transient ischemic attack or stroke. Renal artery involvement is associated with hypertension usually. FMD is discovered after a delay of 4 years when it is focal in nature, and when multi-focal, it may take 9 years after discovery of hypertension to be diagnosed.
Almost 25% of women under 50 years of age suffering from acute myocardial infarction (AMI) have coronary dissection as the underlying cause. Spontaneous carotid or vertebral artery dissection accounts for 20% of strokes in women less than 45 years of age. Dissections may occur in more than 1 artery.
Intracranial FMD most often present as an aneurysm with an estimated prevalence of approximately 7%. There is however little knowledge of long-term prognosis of FMD associated with intracranial aneurysm.
The US registry recorded a higher incidence of dissection and aneurysm in men with FMD albeit there were few men with FMD. There was increased tobacco exposure and early onset hypertension in men with aneurysm. There was no association of tobacco use with dissection.
FMD has been seen in first or second-degree relatives of 75 to 11% patients. A high rate of sudden death and stroke in family members of FMD patients has also been reported suggesting silent dissection and aneurysm. A genetic contribution to FMD is suspected.
Arterial dissection most commonly occurs in the extra cranial carotid and vertebral arteries, with 40% of these patients developing a dissection in more than 1 cervical artery. Importantly, 20% of the family members of patients with dissection had experienced sudden death.
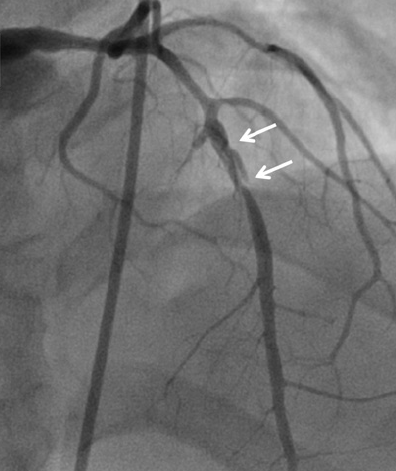
Multiple studies have reported an increased prevalence of FMD in patients who experience coronary artery dissection (45% to 85%), carotid or vertebral artery dissection (20%), or renal artery dissection.
The take home message is that in every patient presenting with sudden death, myocardial infarction, or stroke, it is essential that FMD be kept in mind. There is high prevalence of aneurysm and dissection among patients with FMD. Such patients will need to be imaged with CT or MR angiography form head to pelvis. Efforts have to be made to uncover etiological factors and treatment of FMD.
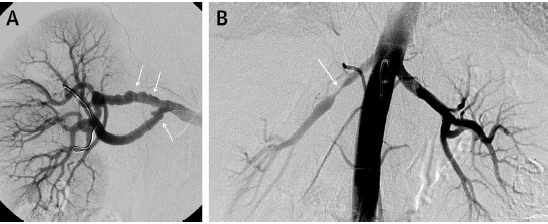
The first report of FMD and spontaneous coronary artery dissection (SCAD) was made in 1965. Clinical presentation of coronary involvement with FMD is uncommon but the true prevalence is unknown. This is is largely due to lack of symptoms before an acute event and pack of specific coronary findings. The string of beads appearance seen in in the renal, carotid, and other arterial beds rarely, if ever, occurs in the coronary arteries. Most patients have smooth coronary arteries or dissection. It is presumed that estrogen may have a role in the etiology of FMD because most patients are women. The consensus is that FMD is a multifactorial disease with varying contributions from genetic, gender/hormonal and environmental influences.
Fibromuscular dysplasia is present in the majority of patients with SCAD, but SCAD may occur in the absence of FMD. Imaging consistent with FMD was seen in more than 86% of patients of non-atherosclerotic SCAD. The US registry has reported that in patients of FMD presenting with SCAD, the carotid arteries were involved in 73%, vertebral arteries in 19%, renal arteries in 16%, and coronary arteries 5%.
Patients with SCAD are predominantly female, with mean age at presentation of 50 years. They usually have no cardiovascular risk factor apart from hypertension. Hormonal changes during pregnancy affect the arterial wall, predisposing possibly to dissection in the presence of increased cardiac output, which occurs throughout pregnancy and especially during delivery.
There are no guidelines laid down for the treatment of SCAD; because of the absence of prospective trials and large observational studies. In stable patients without active myocardial ischemia a conservative approach is preferred. This is because SCAD is capable of healing spontaneously. If stenting is done the dissection flap can extend proximal or distal to the stented segment making matters worse. Stenting is advised in the event of refractory despite optical medical treatment. Dual anti-platelet is given for as year and aspirin thereafter. A beta-blocker is advised with the hope that it reduces coronary shear forces and reduce risk of further dissection.
In unstable patients or those with active myocardial ischemia an interventional approach will be needed. Angioplasty alone is recommended for renal artery FMD, intracoronary stent implantation is usually required for SCAD. Balloon pressures are kept low and stents never sized too large because of the fear of worsening the dissection. IVUS or OCT may help in correct sizing of balloon or stent. Coronary by pass graft surgery is rarely performed in patients with multiple dissection and good distal vessels. There is no clinical evidence for role of statins in non-atherosclerotic SCAD.
There are no data to support or refute use of oral contraceptives or hormonal replacement therapy in FMD with coronary involvement. Hormonal therapy should be used only for compelling reasons. Fibromuscular dysplasia remains an enigma at the molecular and genetic levels. Considerable research is required to unravel the mystery of the genesis of FMD to present an effective and evidence based treatment.