Current guidelines on treating patients with non-ST segment elevation myocardial infarction ( NSTEMI) recommend an invasive strategy because this reduces the risk of death and myocardial infarction ( MI) compared with a conservative or selectively invasive approach. The timing of the invasive strategy still remains controversial. The current European Society of Cardiology guidelines are based on old trials and a meta analysis published in 2013. The TIMACS trial including more than 3000 patients has been the largest trial on the subject to date. The study was stopped prematurely because of difficulty in enrolment and it did not meet its primary endpoint.
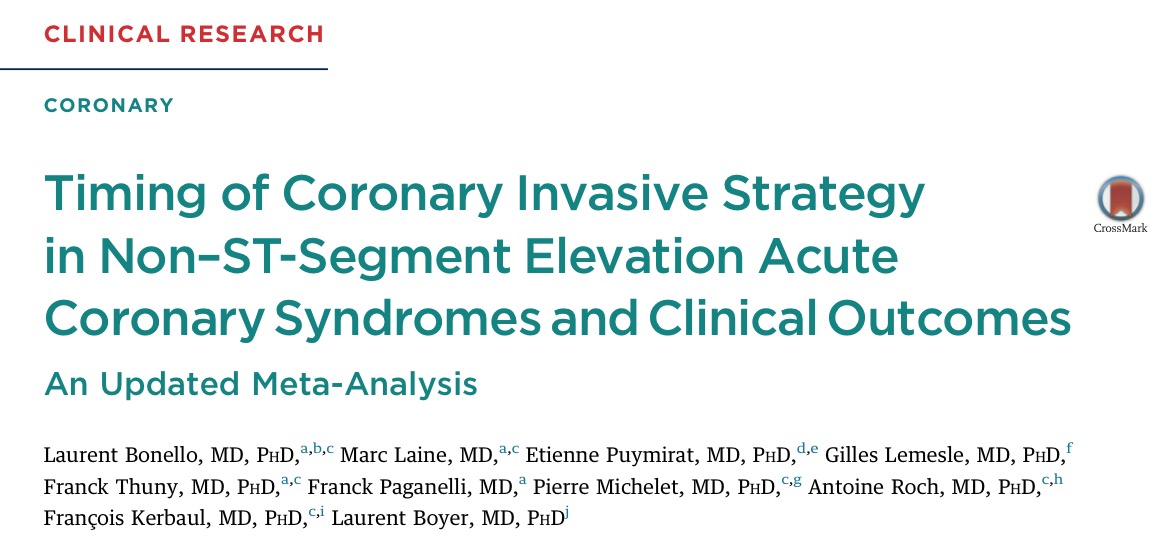
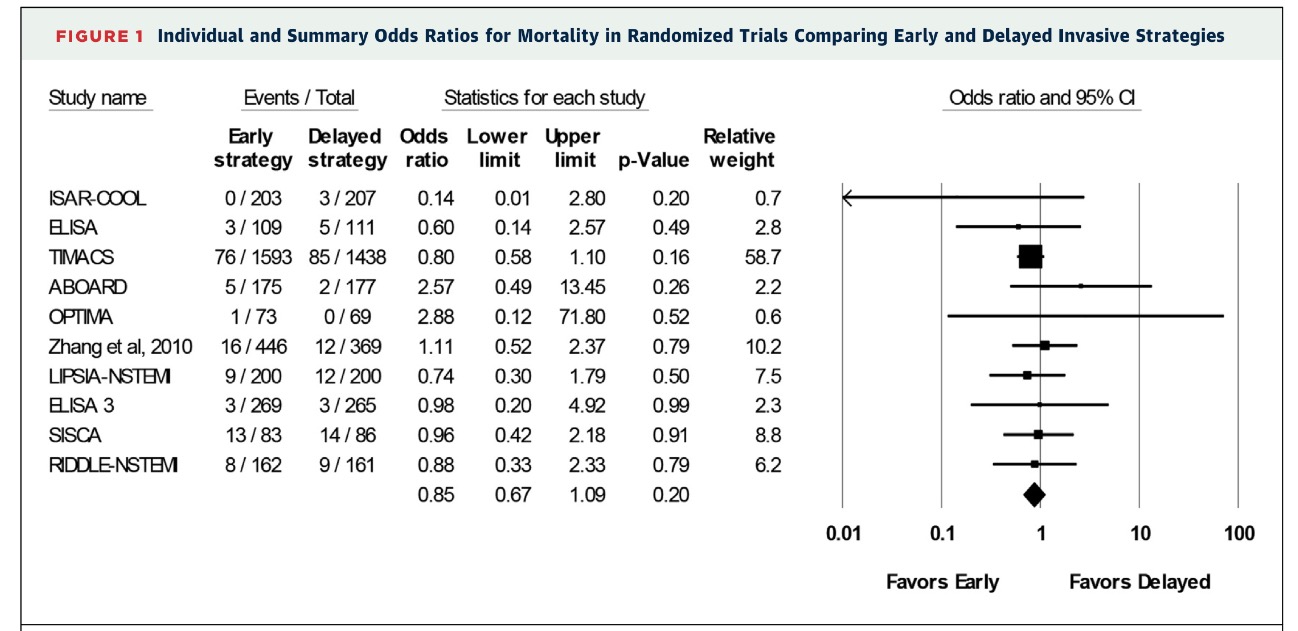
A meta analysis conducted in 2013 that included randomized and observational trials, comparing early invasive with delayed invasive strategies recorded nonsignificant reduction in mortality in the early invasive strategy group in the randomized trials and significant reduction in mortality in the observational data. There was however an increased rate of myocardial infarction in the early strategy group which was not significant.
The most recent meta analysis has added 3 more randomized studies to previous studies in order to better determine timing of intervention in NSTEMI. The median time between randomisation and angiography ranged from 0.5 to 14 hours in the early group, and from 18 to 86 hours in the delayed group. The researchers found in their meta analysis of 10 randomized trials that an early invasive strategy did not result in mortality benefit compared to a delayed approach. It is unlikely that a small delay in intervention would result in increased deaths in patients with NSTEMI ( J Am Coll Cardiol Intv 2016;9:2267-2276).
Both groups had similar rates of myocardial infarction. The meta analysis showed heterogeneity among studies regarding this outcome . Also the definition of MI varied in these studies and often included periprocedural MI, which has no prognostic significance. Crucially in many patients biomarkers did not come down by the time of intervention and therefore it was impossible to rule out index MI from a procedural complication.
Recurrent ischemia (RI) was lowered by a significant 50% by the early invasive strategy. Major bleeding occurred with equal frequency indicating that an early invasive strategy is safe. The aim in a patient with NSTEMI is to stabilise the culprit lesion and arrest the growth of the thrombus and its complications. Early invasive strategy attempts to stabilise the culprit lesion by early revasularisation in combination with antithrombotic therapies. Delayed strategy on the other hand aims to stabilise the culprit lesion using antithrombotic agents as pretreatment to facilitate delayed revasularisation. The meta analysis suggests there is no advantage in a delayed strategy because there is no reduction in mortality or MI, but a higher rate of recurrent ischemia. The ACCOAST trial had concluded that pretreatment with prasugrel in patients with NSTEMI resulted in more bleeds without any benefit in clinical outcome.
Apart from significant reduction in recurrent ischemia, early invasive strategy was associated with shorter hospital stay. Also, patients with a Global Registry of Acute Coronary Events (GRACE) score greater than 140, had significant decrease in the composite endpoint of death,MI and stroke with an early invasive strategy (14% vs. 21%, p=0.006). Very high risk patients are excluded from randomized trials as they need urgent treatment.
Mortlity was similar in both strategies 4% vs. 4.9%, while rates of MI were 6.7% vs 7.7% in early and delayed strategies. Recurrent ischemia or refractory angina was significantly reduced from 5.8% to 3.8%; hospital stay was significantly shortened from a median of 168 hours to 112 hours by the early invasive strategy. Major bleeding was similar; 3.9 vs. 4.2%.
The researchers concluded that there is no difference in death or MI between early and delayed invasive strategies in patients with NSTEMI. An early approach is safe and reduces both refractory angina and hospital stay. It is well to remember that an initial ischemia guided strategy ( delayed approach) often converts to an invasive strategy (signicant spontaneous or inducible ischemia in spite of optimal medical therapy).