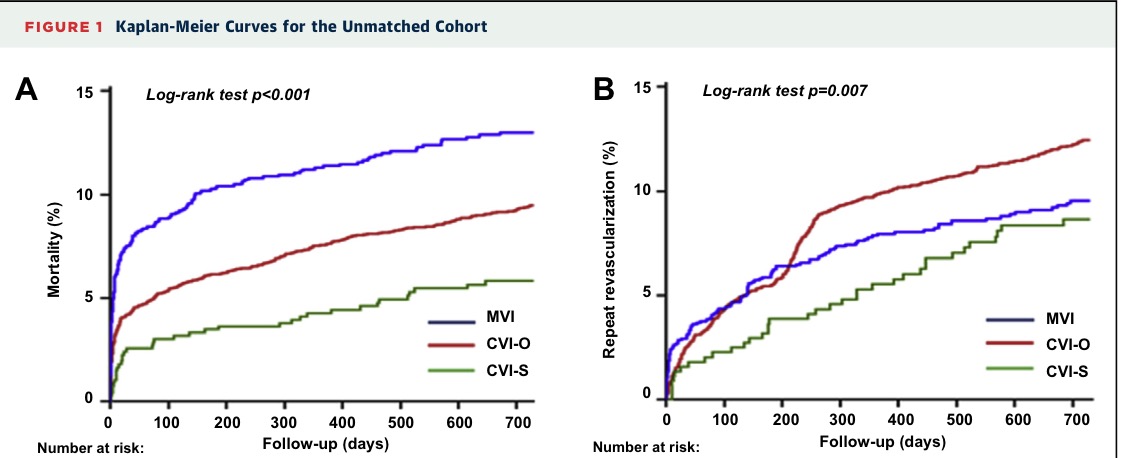
A substantial number of patients presenting with ST elevation myocardial infarction (STEMI) have multivessel disease. The jury is still out whether multivessel intervention ( MVI) during index procedure is superior to culprit vessel intervention only ( CVI-O) during primary percutaneous intervention ( PPCI) in the setting of acute STEMI. A Canadian registry examining more than 6000 patients of STEMI concluded that CVI followed by culprit vessel intervention staged ( CVI-S) had better clinical outcomes than CVI or MVI during index procedure. Coronary artery disease was defined by them as stenosis greater than 70% and multivessel disease as CAD in 2 or more epicardial coronary arteries. CVI-S was found to have lesser mortality than MVI or CVI-O, and lower rates of revascularisation than CVI-O. CVI was associated with better survival in patients more than 60 years, diabetes, renal dysfunction, liver disease and when intra-aortic balloon pump was not required. The authors however conceded that because of the observational nature of their data they could not make specific clinical recommendations. An accompanying editorial praised the details provided as anatomical definitions have been vague in most MVI in patients with STEMI, leading to confusion in accurately recommending a PPCI protocol.
The problems of MVI are coronary microembolization, pronged duration of procedure, greater volume of contrast usage, and iatrogenic myocardial infarction. A recent meta analysis of more than 44,000 STEMI patients did not find reduced death or MI with MVI. MVI did reduce revascularisation as compared to a CVI strategy. Crucially it is difficult to visually or functionally assess non culprit vessels in the acute setting.
The PRAMI trial found MVI in the acute setting was associated with reduced composite end point of death, MI or refractory angina but individual end points did not differ significantly. Similarly individual end points were the same in the CVLPRIT study. No randomised trial has shown significant reduction in mortality with complete revascularisation in the setting of acute STEMI.
Data with acute STEMI accompanied by shock however is clearly in favour of culprit vessel only intervention. At least 5-10% of patients with acute MI present with shock. Mortality is as high as 50% in 30 days in the presence of shock during acute MI. The SHOCK trial done 20 years ago established the superiority of PCI in patients of STEMI accompanied by shock. In the subgroup of patients who underwent MVI or CVI,mortality was significantly greater with complete revascularisation. A meta analysis including more than a 1000 patients with cardiogenic shock reported significantly increased mortality with MVI as compared to CVI (38% versus 29%, p =0.001).
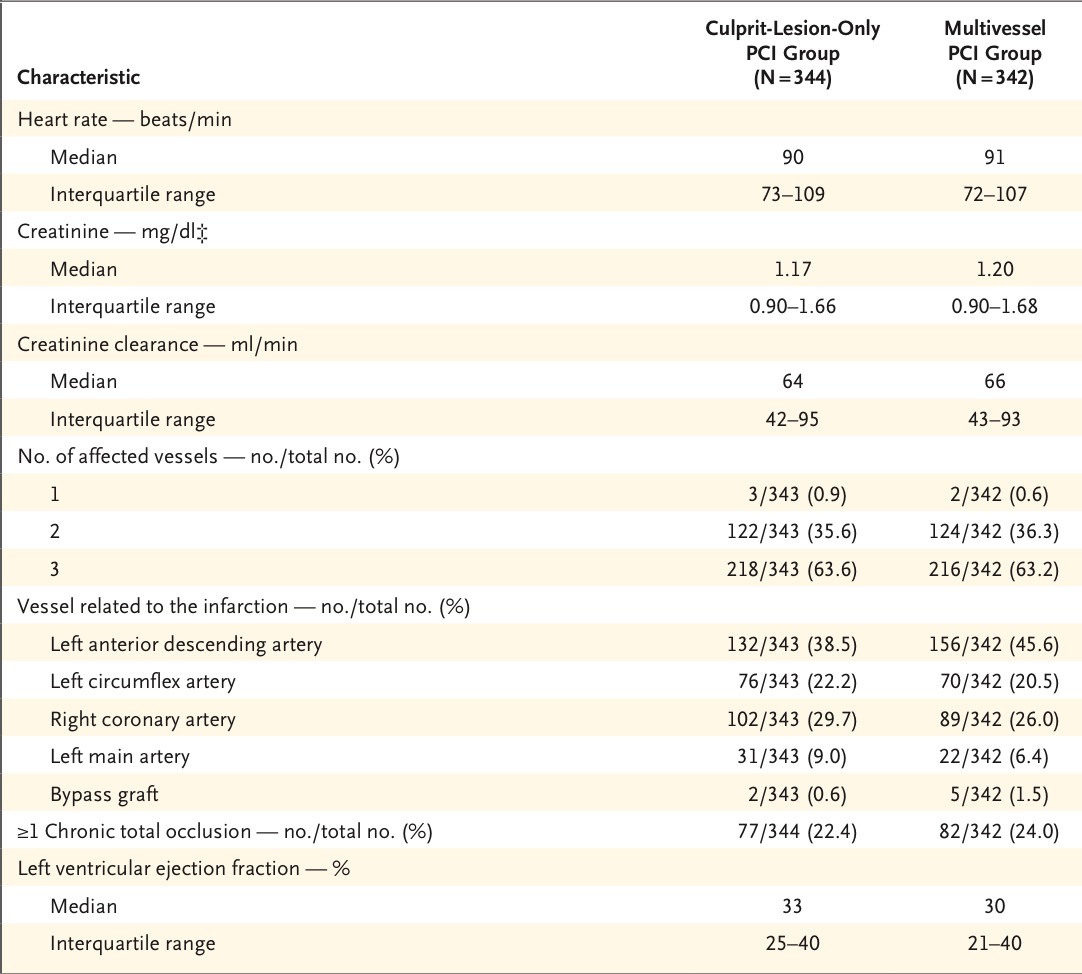
Mortality is substantially increased in patients of STEMI with multivessel disease and shock and the best management strategy so far seems to be intervention of the culprit artery. Most if not all data comparing multivessel intervention with single vessel intervention has been in patients of STEMI without shock. Clinicians therefore need to examine the CULPRIT SHOCK trial carefully. European guidelines encourage non culprit intervention while American guidelines are silent on the issue. Appropriate Use Criteria however recommended non culprit vessel PCI if shock persists after treating the culprit artery. Shock is defined as blood pressure less than 90 mm Hg for at least 30 min , need for catecholamines to maintain blood pressure at 90 mm Hg, clinical signs of pulmonary congestion, at least one sign of organ hypoperfusion ( altered mental status, cold clammy skin, urine output less than 30 ml per hour, or arterial lactate level more than 2 mmmol per litre.
The problems of MVI are coronary microembolization, pronged duration of procedure, greater volume of contrast usage, and iatrogenic myocardial infarction. A recent meta analysis of more than 44,000 STEMI patients did not find reduced death or MI with MVI. MVI did reduce revascularisation as compared to a CVI strategy. Crucially it is difficult to visually or functionally assess non culprit vessels in the acute setting.
Data with acute STEMI accompanied by shock however is clearly in favour of culprit vessel only intervention. At least 5-10% of patients with acute MI present with shock. Mortality is as high as 50% in 30 days in the presence of shock during acute MI. The SHOCK trial done 20 years ago established the superiority of PCI in patients of STEMI accompanied by shock. In the subgroup of patients who underwent MVI or CVI,mortality was significantly greater with complete revascularisation. A meta analysis including more than a 1000 patients with cardiogenic shock reported significantly increased mortality with MVI as compared to CVI (38% versus 29%, p =0.001).
Recently a randomized trial assigning STEMI or non STEMI patients with cardiogenic shock to culprit vessel only and multivessel intervention ( in 70% or more stenosis of non culprit vessels) has also reported greater mortality with the latter. The major end point of death or severe kidney failure needing replacement therapy was significantly greater with multivessel intervention. The CULPRIT SHOCK trial has further buttressed the policy of culprit vessel only PCI instead of aiming for complete revascularisation. Shock is a lethal situation in the setting of STEMI due to heightened platelet reactivity consequent to catecholamines, pro thrombogenecity and inflammatory state as a result of shock itself. Mortality with CVI only was 45% at 30 days. Additional trials are required to assess other strategies for lowering mortality in STEMI accompanied by shock. Patients with left main disease or diabetes with multivessel disease undergoing CABG had similar mortality to culprit vessel only intervention. Mortality was increased with ECMO ( extracorporeal membrane oxygenation ) use in multiple vessel intervention in the CULPRIT SHOCK trial. The role of ECMO needs to be established by randomized studies. It must be noted that in the CULPRIT SHOCK trial death or severe renal failure was reported in 45% of patients at 30 days with culprit vessel only PCI as opposed to 55% with multivessel stenting.
The CULPRIT SHOCK trial authors concluded that in the setting of cardiogenic shock culprit artery PCI is superior to multivessel PCI, due to significantly lower mortality with the former approach. The researchers theorised that greater use of contrast in multivessel intervention results in greater kidney injury as also cardiac volume overload.