
There is unanimous agreement that intervention is needed once a patient with severe valvular aortic stenosis (AS) becomes symptomatic. Valvular AS is not uncommon in the western world with a prevalence as high as 3 % in people over 70 years. Prevalence amongst Indians is unknown but no where near the Western statistic. Te usual risk factors associated with atherosclerosis are linked to aortic stenosis but so far no method for prevention has been identified. Nor is anything known about arresting progression of mild AS to severe AS.
Severe AS is defined as a mean gradient across the aortic valve greater than 40 mm Hg, peak flow on Doppler echo more than 4 m/sec, or valve area less than 1 cm2. The 3 key symptoms associated with severe AS are angina, syncope and dyspnea. Life span is considerably shortened once symptoms set in and may be as short as 2 years with onset of breathlessness. It should be remembered that incidence of sudden death hovers around 1-1.5% per year.
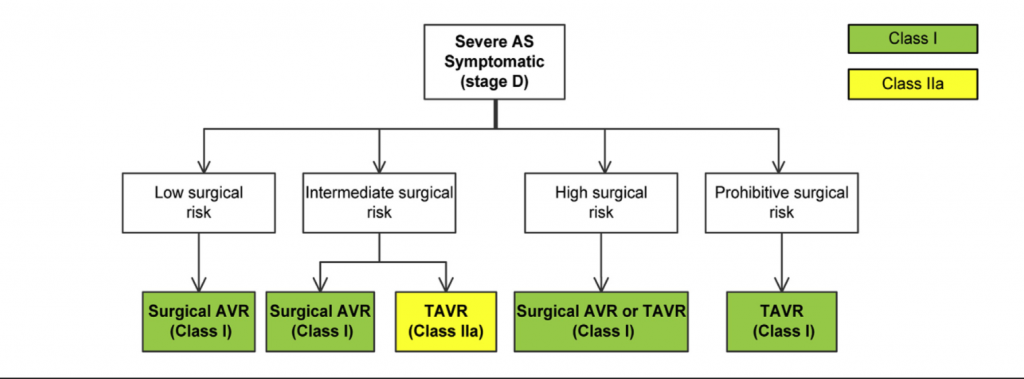
Currently surgical aortic valve replacement (SAVR) carries mortality as low as 1 to 2% in most experienced centres. Transcatheter aortic valve replacement (TAVR) has over the years become an established alternative to SAVR in a substantial number of cohorts. There is no significant difference in mortality between SAVR and TAVR I patients with both high risk and intermediate risk patients with AS. Surgical risk for AS is anticipated best with the Society of Thoracic Surgery (STS) Risk Score. A predicted risk score by STS of 4% to 8% mortality (by 30 days) is considered intermediate risk, an STS more than 8% is high surgical risk, while less than 4% is low risk. Randomised trials in intermediate risk and high risk patients have confirmed that TAVR is equivalent to SAVR. There were more vascular complications and pacemaker implantation with TAVR, while SAVR was linked with more need for blood transfusion, acute kidney injury and atrial fibrillation. A small Nordic study has demonstrated equivalence between TAVR and SAVR in patients with low risk also, but larger randomiser trials obviously need to confirm this. Contemporary guidelines recommend that patients with intermediate and high risk can be offered both SAVR and TAVR. Patients with very high operation risk (‘inoperable’) should be offered TAVR instead of SAVR, and patients with low risk undergo SAVR for now.
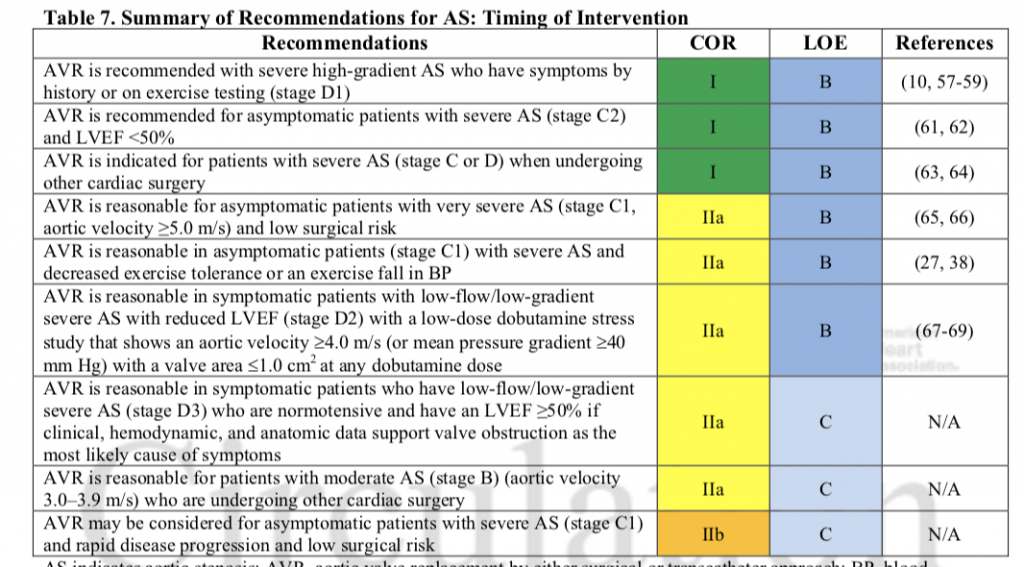
Aortic valve replacement (AVR) is also recommended for asymptomatic AS patients with an LVEF less than 50% ( mean gradient 40 mm Hg, peak aortic flow >4 m/sec) ( Recommendation Class 1, Evidence Level B).
AVR is also recommended in asymptomatic AS patients undergoing some other cardiac surgery (CABG for example) provided there is evidence of severe AS (in the form of mean gradient more than 40 mm Hg, peak aortic flow more than 4 m/sec)(Recommendation Class 1, Evidence Level B).
AVR is recommended for asymptomatic patients with with “very severe” AS if the peak flow is more than 5 m/sec ( Recommendation Class II a, Evidence Level B)
AVR is recommended (Class II a, Evidence Level B) in symptomatic patients with severe AS who have fall in systolic pressure during a stress stress or decreased exercise tolerance.
Next we have a very interesting group of patients classified as the “low flow/ low gradient” severe AS considered for SAVR or SAVR; these patients have to be symptomatic. The first subtype are those patients with reduced systolic left ventricle function, low LV ejection function (< 50%). These patients apart from calcified aortic leaflets with reduced mobility have a mean gradient less than 40 mm Hg and peak aortic flow less than 4 m/sec. They have a valve area of 1 cm2 or less. These patients when subjected to low dose dobutamine stress study demonstrate an aortic velocity > 4 m/sec or mean pressure gradient greater than 40 mm Hg with a valve area 1cm2 or less at any dose of dobutamine ( Class II a, Evidence Level B).
The other subtype of “low flow/ low gradient” symptomatic severe AS patients have a normal LVEF. These are usually elderly hypertensive women with a hypertrophied small cavity left ventricle. These patients also should have a mean gradient , 40 mm Hg or peak aortic flow > 4 m/sec accompanied by an aortic valve area of 1cm2 or less or indexed aortic valve area of 0.6 cm2/m2 or less; and a stroke volume of 35 ml/ m2 ( Class IIa, Evidence Level C)
Physicians have begun to mull over earlier intervention in patients with severe AS, even going to the extent of recommending surgery in patients without symptoms. The reason is that symptoms are not recognised by a number of patients. Also accompanying co-morbity tend to confuse both patients and treating physicians regarding their symptoms. There is a case for identifying biomarkers to tease out asymptomatic patients of severe AS who would benefit from intervention. A recent British paper on this subject is bound spark considerable discussion on whether a change in timing of intervention is overdue.

This paper not only describes the various forms of myocardial fibrosis( MF) picked up by cardiac magnetic resonance imaging (CMR) employing late gadolinium enhancement (LGE) , but goes on to suggest MF is linked to substantial increased mortality in patients with severe AS undergoing AVR. The use of CMR to identify patients requiring AVR may not enter routine decision making but must certainly be food for thought. The British registry included 674 symptomatic patients with severe AS who underwent SAVR or TAVR following a CMR evaluation. The remarkable observations noted in this study are that myocardial fibrosis occurs in as many as 51% of severe AS patients, two thirds of MF are reactive while one third are due to myocardial infarction. Reactive fibrosis is patchy and reversible , while MF due to myocardial infarction is irreversible, extending from sub-endocardium to epicardium. Patients with MF tend to have greater LV hypertrophy, lower ejection fraction and more symptoms. Worse MF regardless of type was linked to three fold (15% versus 5%) increase in mortality over a median follow up of only 3.6 years, whether SAVr or TAVR was performed. The adverse effect of fibrosis was not binary but graded; all cause mortality increasing 11% for every 1% increase in MF.
We now have the tantalising prospect of picking up patients of severe AS for intervention by CMR before myocardial fibrosis sets in. Adequately powered randomised trials are urgently needed to better elucidate the prognostic role of myocardial fibrosis.