The STICH trial, published 5 years ago, randomly assigned 1212 patients with an ejection fraction of less than 35% and coronary disease amenable to coronary-artery bypass grafting (CABG) to receive optimal medical therapy for heart failure and coronary artery disease (602 patients) or to receive optimal medical therapy and CABG. There was, after 5 years of follow up, no significant difference in death from any cause. Surprisingly, in a sub-study, assessment of myocardial viability failed to show any patient that may have benefited from CABG. No patient had >50% left main coronary artery stenosis or Canadian Cardiovascular Society class III-IV angina.
The patients had mean age of 60 years, more than 60% had angina, and more than 60% of patients were in New York Heart Association functional class II or I heart failure. We now have a further 5 years follow up of these patients published once again in the NEJM last week. The primary outcome was death from any cause. The secondary outcomes included death from cardiovascular causes and death from any cause or hospitalization for cardiovascular causes. The median duration was 9.8 years.
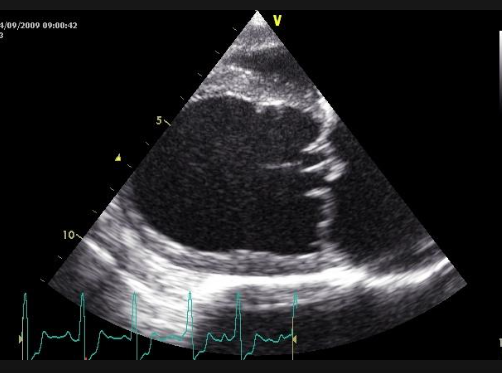
A primary outcome event occurred in 59% in the CABG group versus 66% in the medical therapy group. Death from cardiovascular causes was seen in 41% in the CABG group versus 49% in the medical therapy group. The researchers concluded that in patients with ischemic cardiomyopathy, rates of death from any cause or cardiovascular causes were significantly less with CABG. The STICH Extension Study (STICHES) achieved a 98% rate of follow up in 1212 patients. Internal mammary artery grafting was used in 91% of CABG patients while 30-day CABG mortality was 3.6%. Almost 40% patients had diabetes, 77% had had a previous myocardial infarction, and 86% had New York Heart Association functional class II to III heart failure. The average left ventricle ejection fraction in the viability subgroup was 27% study involving 601 patients. The ejection fraction in the non-viable patients was as low as 23%. The all cause mortality advantage of CABG over medical therapy , which surfaced 3 years after treatment, was present in multiple clinical subgroups.
The American Heart Association provides a recommendation of IIb (2012 guidelines) for CABG in patients with severe left ventricle dysfunction (ejection fraction <35%), based largely on the earlier STICH data. Crucially viability was not found to have any interaction with CABG benefit. The STICHES trial has demonstrated 1.4 median extension of survival. It would be reasonable to advise CABG to a 60-year-old man with an ejection fraction of 30% and NYHA class III heart failure. A different patient let us say with age of 70 years, previous CABG, ejection fraction of 30%, creatinine of 2.2 mg%, moderate mitral regurgitation would be a difficult choice for CABG.
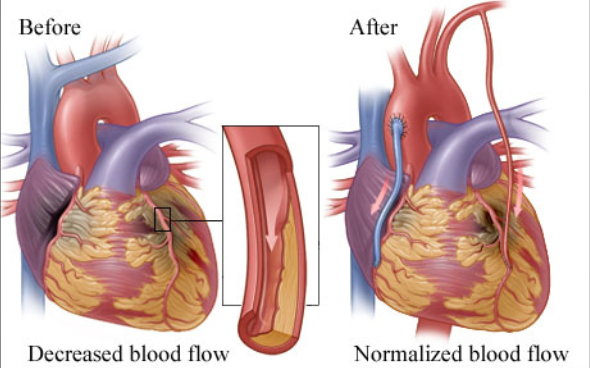
It must be emphasized that percutaneous coronary intervention would also be an alternative, particularly if the SYNTAX score were less than 22. The STICHES data however makes a strong case for CABG in patients of ischemic cardiomyopathy with ejection fraction less than 35%. But we should be always looking for newer ideas and other alternatives in the management of such patients. Surprisingly, the STICHES researchers have not provided any data on change in the left ventricle ejection fraction in either group of patients nor have they been able to explain the improvement in survival of these patients.
The STICHES trial supports the original hypothesis that CABG may offer a survival benefit to patients with severe coronary artery disease and left ventricle dysfunction. Crucially, almost 60% patients in the CABG group died in 10 years making it mandatory that the search for effective treatment for patients with ischemic cardiomyopathy is vigorously continued with.