
Millions across the globe suffer form congestive here failure with enormously high rates of morbidity and mortality. A significant proportion of deaths are due to sudden death despite the best guideline based treatment. Crucially in numerous patients with dilatation of the left ventricle the mitral annulus dilates, disallowing optimal coaptation of mitral leaflets. The enlarging heart pulls the valve apart.The altered architecture of the mitral valve apparatus results in regurgitation of blood into the left atria further aggravation the situation. Patients feel exhausted, and hit a stage where they can barely walk a room’s length. They also get short of breath on slightest exertion, worse they are breathless even when they attempt to sleep. They often have to sit up during nights in order to catch their breath. The failing heart tries to compensate by expanding but this only makes matters worse, by increasing the leak (or regurgitation ) across the mitral valve.
It is still unclear whether mitral regurgitation is a sequel of the failing and enlarging left ventricle or whether it actually contributes to the pathophysiology of congestive heart failure. Mitral regurgitation subsequent to a failing left ventricle is termed secondary mitral regurgitation (earlier called functional regurgitation). Surgical intervention in the form of mitral valve replacement or surgical repair has not altered prognosis so far. Degenerative or primary mitral regurgitation, on the other hand can be treated with surgical valve replacement or valve repair.
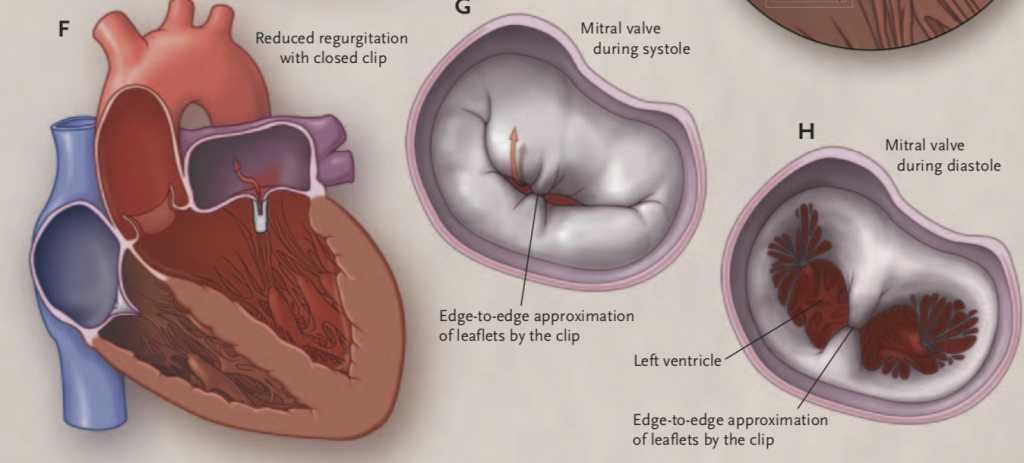
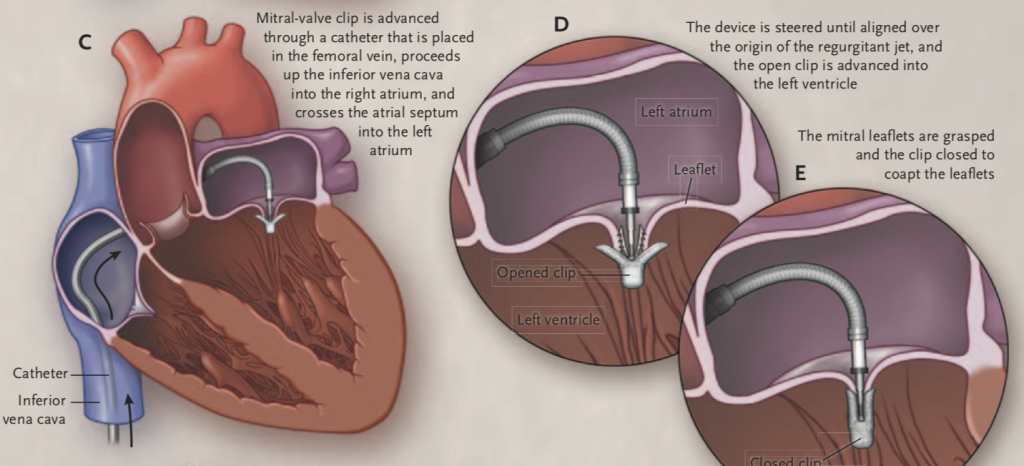
Recently 2 randomised trials using the mitral clip have been published with diametrically opposite clinical results. It is a matter of concern that 2 studies published within a month of each other provide different clinical outcomes. The French MitraClip randomised trial got published first. It should be emphasised that strictly speaking the trial was not blinded because the clip can be seen on 2D echocardiography. The MitraClip is a device that clips the 2 cusps of the mitral valve to reduce the leak. This was called the edge to edge repair and has been done surgically during open heart surgery. The MitraClip is based on the principle of surgical edge to edge repair, but this device is impacted by attaching it to the end of a catheter, which is inserted via the femoral vein in the groin. Under fluoroscopy guidance the device is threaded up the femoral vein into the right atrium and from there into the left atrium by means of puncturing the inter atrial septum. The mitral leaflets are clipped using an echocardiographic probe positioned in the oesophagus (close to and right behind the heart) and fluoroscopy ( X Ray) guidance.

The EVERST II investigators had earlier shown in a randomised manner that in patients with moderately severe or severe (grade 3+ or 4+) mitral regurgitation, percutaneous repair, albeit less effective than conventional surgery in reducing mitral regurgitation, was associated with similar clinical outcomes and better safety ( N Engl J Med 2011;364: 1395). The study is 7 years old and there has been considerable improvement in the hardware plus skills of the operator. The 5 year follow up reported that surgery was needed in the MitraClip group for residual mitral regurgitation in the first year, but by 5 years there was no significant difference in mortality and both the clip and surgery displayed equal reduction in regurgitation ( J Am Coll Cardiol 2015; 66:2844-54).
Now we have another North American trial in which 614 patients with severe heart failure were assigned to a MitraClip and standard medical treatment or standard treatment alone (N Engl J Med Sep 23, 2018) . By 2 years only 92 patients were hospitalised in the MitraClip group, while 28 died. In contrast there were 151 cases needing hospitalisation for heart failure and 61 died. Death from any cause occurred in 29% of MitraClip patients as opposed to 46% in the control group. Annualized hospitalisation was 36% with MitraClip and 68% in controls. The researchers concluded that device based treatment in patients with heart failure accompanied by moderately severe to severe secondary mitral regurgitation, ( who remained symptomatic despite maximum guideline directed treatment) resulted in significantly less death and hospitalisation for her failure.
The North American trial (COAPT) trial came close on the heels of a MitraClip French trial ( N Engl J Med 2018;, that had shown no difference in mortality or hospitalisation for heart failure in more than 300 patients of heart failure with secondary mitral regurpitiuon defined as regurgitant volume more than 30 ml per beat or an effective regurgitant orifice area of > 20 mm2, and left ventricular ejection fraction 15 and 40%. At 2 years primary outcome (death or heart failure hospitalisation ) was 55% in the device group and 51% in medically treated patients. Rates of death were 24% and 22% , while rates of heart failure were 49% and 47% respectively. The authors reported that death or hospitalisation for heart failure did not change at all with the MitraClip. The mean LV ejection fraction was 33%, the mean effective regurgitant orifice area was 31 ml2 and mean regurgitant volume was 45 ml, in both groups. Complication rate in the MitraClip group was around 10%, with a seven fold increase in stroke.

The mean LV ejection fraction in COAPT (American) is 31% while the effective regurgitant orifice area is 41%. But 20% of patients had an ejection fraction greater than 40%. Remember no patient had an ejection fraction more than 40% in the French trial, which reported no improvement in clinical outcomes with the MitraClip. It is indeed difficult to reconcile these polar opposite trial results. One null while the other being stunningly positive.
The difference in clinical outcomes in these 2 trials could be because in COAPT surprisingly more patients in the device group were treated with ACE inhibitors and angiotensin receptor blockers, this is acknowledged by the researchers themselves. Also one fifth of patients in COAPT had an ejection fraction more than 40%, this could contribute to better outcomes than the French trial. It is a moot point whether better outcomes in COAPT were because of better patient selection, and better operating skills. The effective regurgitate orifice area though was indeed more in COAPT than the French trial. The French trial was largely funded by the government while in America funding was entirely by the manufacturer. Moreover royalties of sale of MitraClip went to Columbia University, of which the principal investigator of COAPT is a faculty member.
In view of the contradictions, we clearly must wait for the next big MitraClip randomized trial ( RESHAPE-HF2 ) to be presented. Till then common sense dictates that we bear in mind the potential efficacy of the MitraClip in treating patients of heart failure with severe mitral secondary regurgitation. We now can grapple with the tantalising possibility that a leaking mitral valve contributes in the pathophysiology of heart failure, that secondary mitral regurgitation is not merely a bystander or entirely secondary to a flaccid enlarging heart.
So we have an industry sponsored study showing significant reduction in death, and heart failure hospitalisation, apart from improved quality of life. The company was involved in site selection and data analysis. In fact , the trial has shown that only 3 patients are needed to be treated for 2 years to prevent hospitalisation and only 6 are required to be treated by this clip for 2 years to prevent mortality. A spectacular result by any standards; there are more than 50 lakh ( 5 million) heart failure patients in the US alone. But the cost of the MitraClip is 30,000 $, not including cost of the procedure or doctor/staff fees. However a French study on the same clip failed to show any improvement or difference in clinical outcome in heart failure patients accompanied with severe mitral regurgitation. The French study was mostly funded by their health ministry although the clips were provided by the company. Ultimately one will have to tease out the subset of patients who stand to benefit most by the MitraClip, till the RESHSAPE-HF2 data comes in.