By Deepak Natarajan
Monday, November 28, 2011
Operator(s):
Deepak Natarajan, Mafooza Rashid, Betshiba Dinaker, Vijeta Maheshwari, Nirmalya Mukherjee.
Affiliation:
Cardiological Society of India.
Facility:
Department of Interventional Cardiology
Moolchand MedCity, New Delhi, India
History:
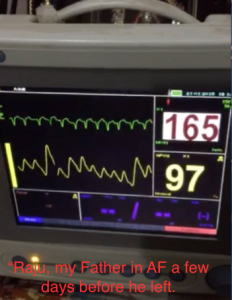
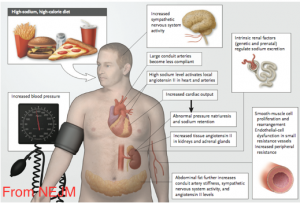
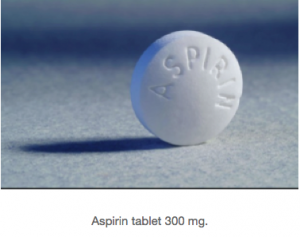
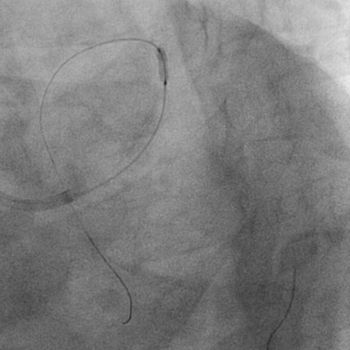
A 52 year male who was a chronic smoker was admitted for severe crushing retrosternal chest pain accompanied by nausea and perspiration for the previous 4 hours. He had no previous history of hypertension or diabetes. On examination in the ER he had a heart rate of 62-66 per minute, blood pressure 130/76 mm Hg, a fourth heart sound on auscultation, but no cardiac murmur. His chest was clear. His ECG revealed an acute infero-lateral myocardial infarction (Figure 1).The patient was given 325 mg aspirin, 600 mg clopidogrel and 5000 units heparin.
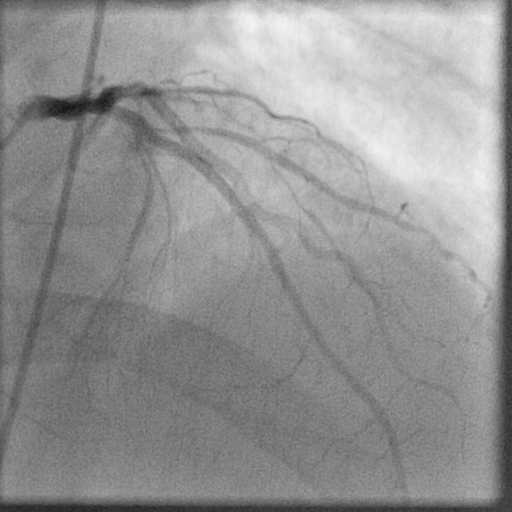
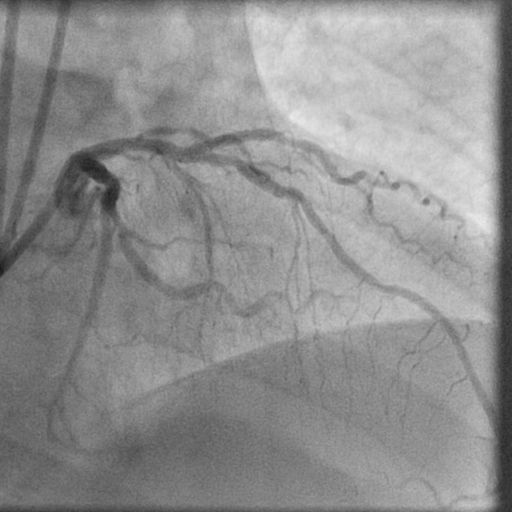
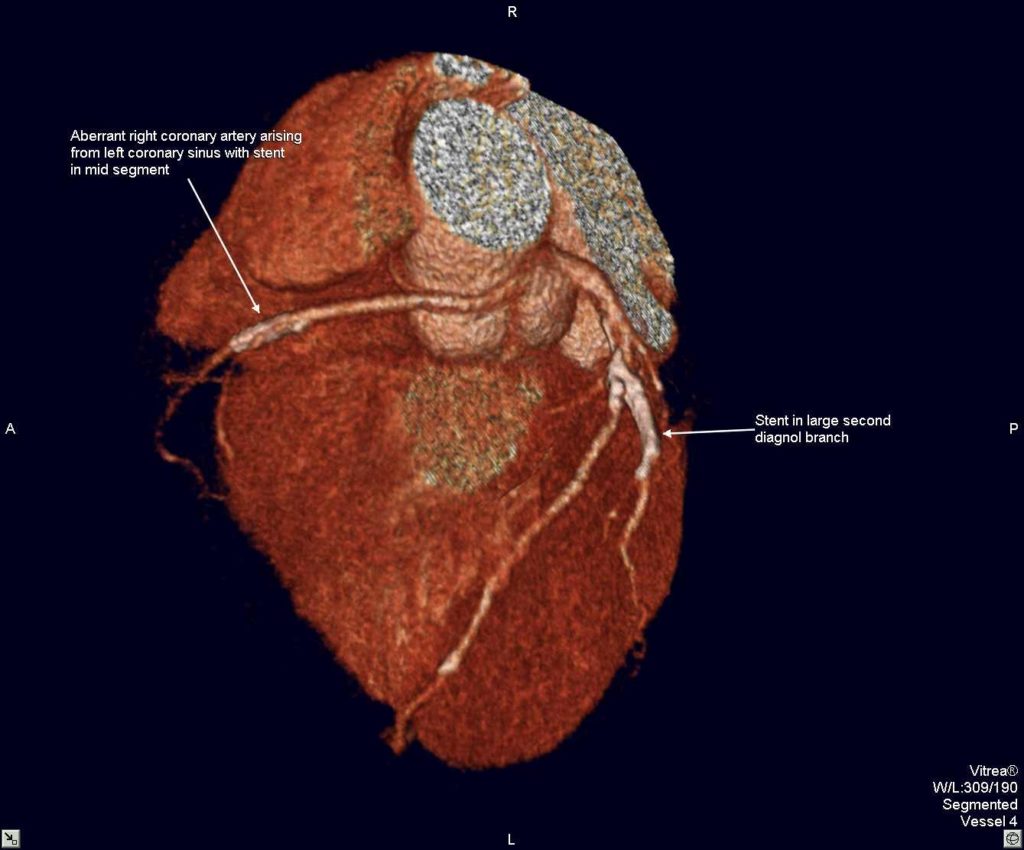
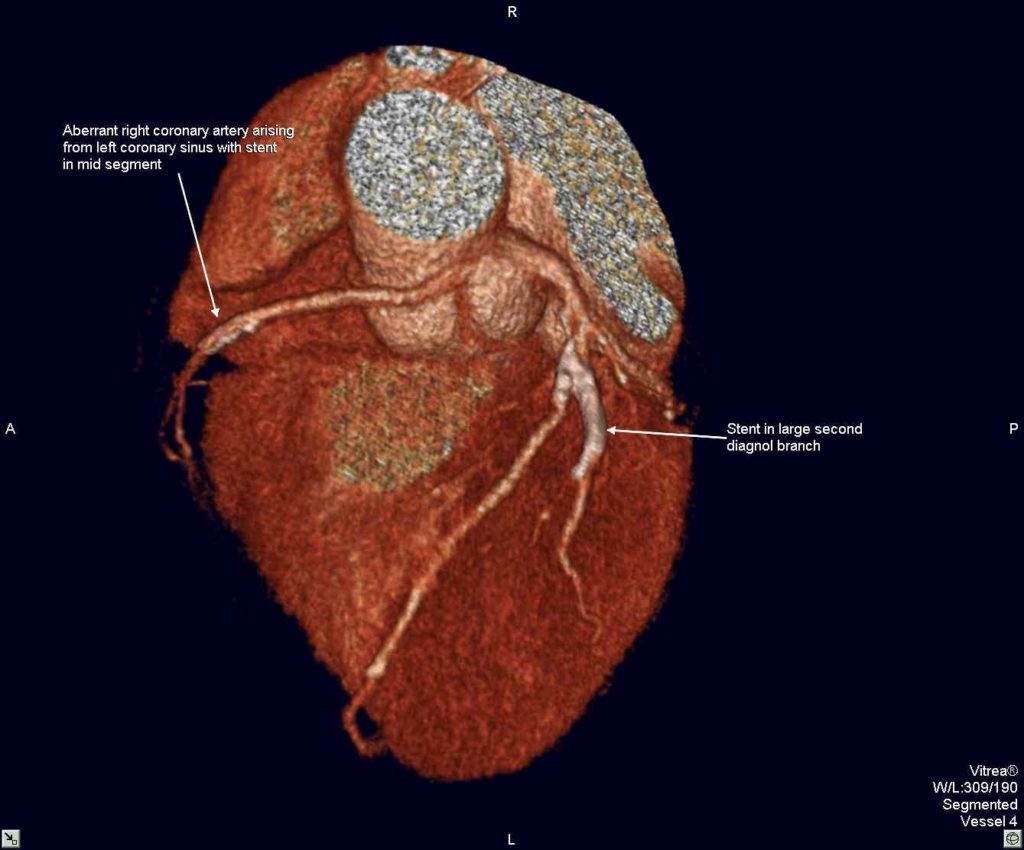
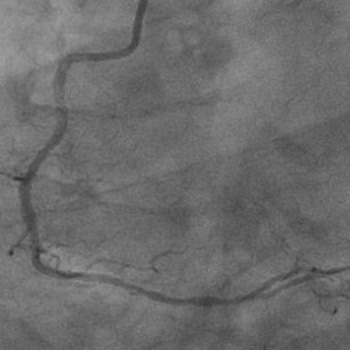
Angiography:
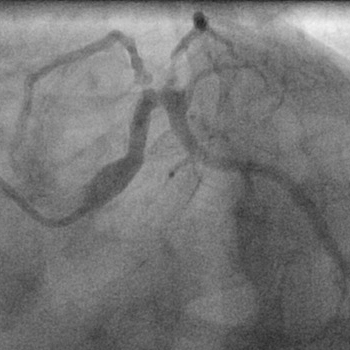
1) LAD: Normal
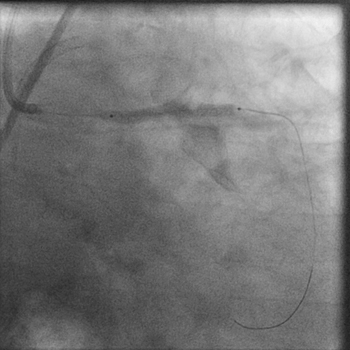
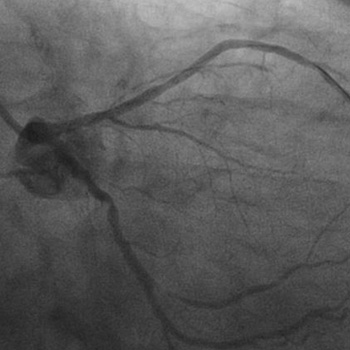
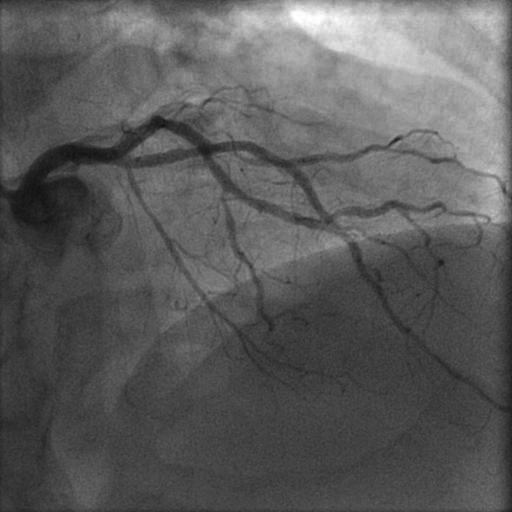
2) LCX: 80% stenosis proximally (figure 2).
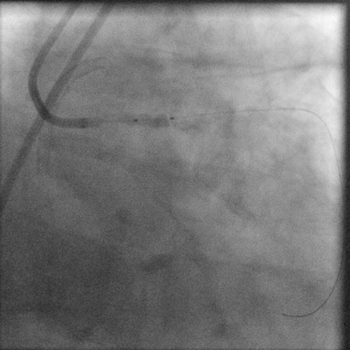
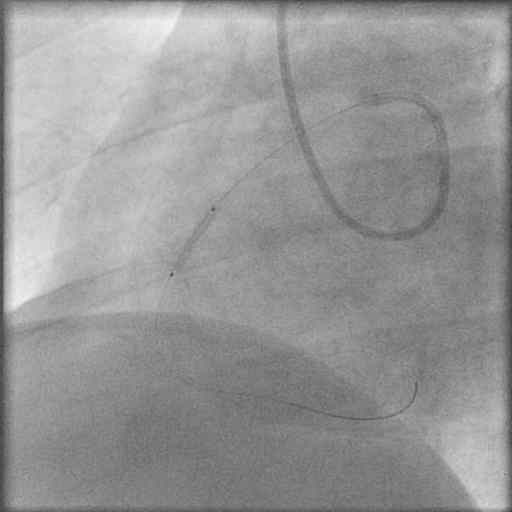
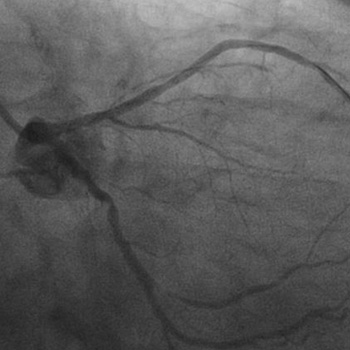
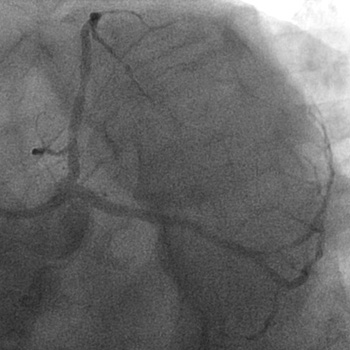
3) RCA: 100% mid occlusion (figure 3)
Procedure:
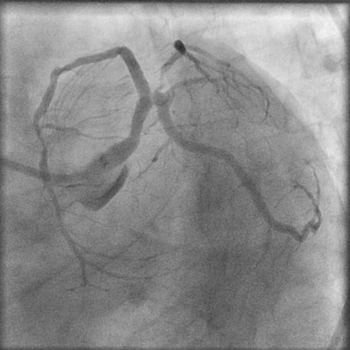
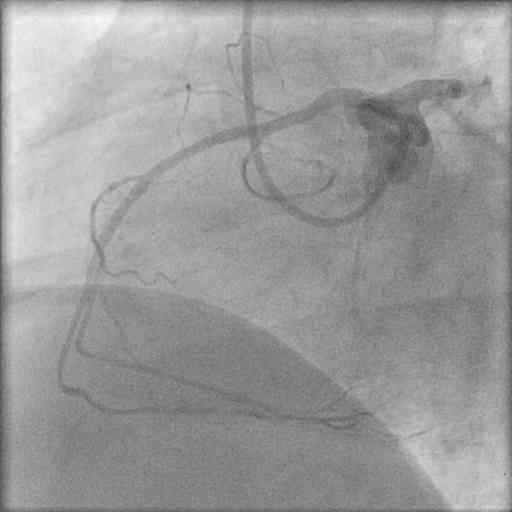
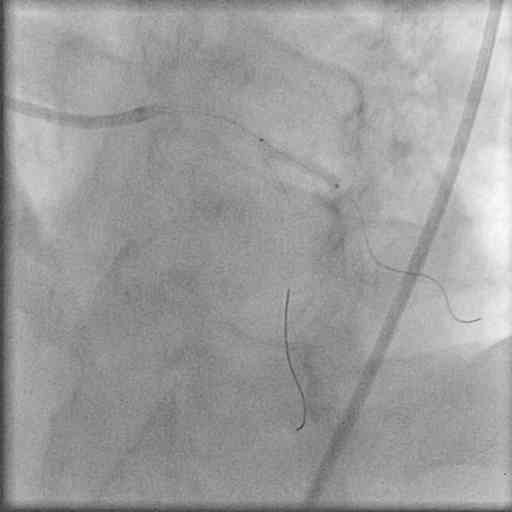
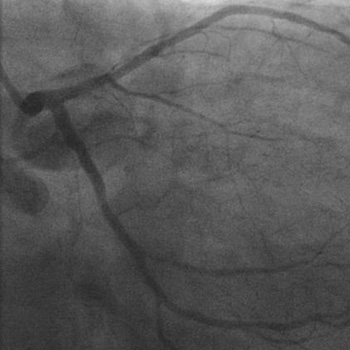
The RCA was engaged with a JR 6Fr guiding catheter, and a 0.014″ floppy guidewire was used to cross the occlusion. After pre-dilation with a 2×10 mm balloon and intracoronary administration of 25 mcg/Kg of tirofiban, a 2.75x18mm bare metal stent was deployed at 16 atm with excellent antegrade flow and no residual stenosis (figure 4). The patient, however, continued to be restless and in pain. It was decided therefore to tackle the LCX lesion in the same sitting. The left coronary artery was engaged with a 6 Fr EBU guiding catheter, the same floppy guidewire used for the RCA intervention was positioned in the distal LCX, and the LCX lesion was predilated using a 2x12mm balloon(figure 5). Because the result was not satisfactory, 2.5x10mm balloon was introduced into the guiding catheter over the floppy guidewire. It was suddenly observed that the pressure wave was getting damped, and the systemic pressure was rapidly dropping (figure 6). Angiography demonstrated massive air embolism in both LAD and LCX arteries with no contrast flow beyond the mid segments of both arteries (figure 7). The patient was pulseless with electromechanical dissociation (figure 8). The balloon that was still in the guiding catheter was rapidly removed, and an attempt was made to suck out the air from the left coronary arteries via the guiding catheter. There was absolutely no improvement. Therefore, the guiding catheter was disengaged, and cardiopulmonary resuscitation (CPR) initiated with vigorous external cardiac massage (figure 9, figure 10). The patient was given 100% oxygen.The patient by now had received 2 IV atropine injections and was also put on IV dopamine. External cardiac massage was maintained for almost 4 minutes by which time the patient recovered both his heart rate and blood pressure. After ascertaining that the patient was hemodynamically stable (figure 11) and had fully recovered his consciousness, the LCX was stented with a 3x18mm sirolimus eluting stent at 14atm. (figure 12) with TIMI 3 flow and no residual stenosis (figure 13).
Conclusion:
The patient was asymptomatic by the time he was moved to the coronary care unit, and his ECG showed almost complete resolution of the elevated ST segments seen prior to the procedure (figure 14). The patient was discharged after 48 hours.
Comments:
Coronary air embolism, albeit rare (incidence ranging from 0.2%- 0.8% during percutaneous interventions) can have a heterogenous presentation ranging from mild symptoms to cardiac arrest and death. Air can be introduced inadvertently by inadequate aspiration of the guiding catheters, rupture of balloons, and leakage of air via a defective manifold system. The management of massive air embolism as seen in this case has to be extremely quick with 100% administration of oxygen to drive out the nitrogen from the air bubbles along with supportive measures such as CPR with emphasis on external cardiac massage. Aspiration and also forceful injection of contrast has been recommended. Aspiration did not work in this case, and forceful injections or manipulation of the guidewire were avoided because of the fear of traumatizing the left main, LAD, or LCX arteries. Aspiration with the Export catheter has also been described in a case report. Coronary air embolism during coronary angiography or PCI should be prevented by careful emphasis on good techniques during the procedure. Treatment has to be rapid and should consist of 100% oxygen accompanied by CPR, DC cardioversion, and if needed IABP.
Conflict of Interest:
None